Orginal Research
2023
June
Volume : 11
Issue : 2
Post COVID-19 mucormycosis- histopathology and associated factors
Patil S, Khade M, Agrawal S, Agrawal S, Kangate S, Sarate D
Pdf Page Numbers :- 81-85
Suwarna Patil1, Manjiri Khade1, Shobhana Agrawal1, Shailesh Agrawal2,*, Swarada Kangate1 and Dilip Sarate1
1Department of Pathology, Government Medical College, Akola, Maharashtra 444001, India
2Department of TB and Chest, MGM Medical College, Indore, Madhya Pradesh 452001, India
*Corresponding author: Dr. Shailesh Agrawal, Assistant Professor, Department of TB and Chest, MGM Medical College, Indore, Madhya Pradesh 452001, India. Email: shailesh.indori@gmail.com
Received 17 November 2022; Revised 3 March 2023; Accepted 10 March 2023; Published 17 March 2023
Citation: Patil S, Khade M, Agrawal S, Agrawal S, Kangate S, Sarate D. Post COVID-19 mucormycosis- histopathology and associated factors. J Med Sci Res. 2023; 11(2):81-85. DOI: http://dx.doi.org/10.17727/JMSR.2023/11-16
Copyright: © 2023 Patil S et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: SARS-COV-2 infection (COVID-19) may be associated with wide range of bacterial and fungal infections. Mucormycosis is a common and potentially life threatening opportunistic fungal infection responsible for morbidity and mortality. Many factors like diabetes mellitus, hypertension and corticosteroid therapy might have been a role in the immunocompromised state of the patients. The aim of present study was to know the predisposing factors and role of histopathology in diagnosis and assessing the prognosis of post COVID-19 mucormycosis cases.
Material and methods: It is a prospective observational study conducted in tertiary care hospital over a period of 6 months from April 2021 to September 2021. Functional endoscopic sinus surgery (FESS) and maxillectomy samples from 157 post COVID-19 mucormycosis suspected cases were studied and details regarding history of diabetes mellitus, hypertension and corticosteroid therapy were retrieved. All tissue samples were examined under H&E stain and special fungal stain (PAS).
Results: On histopathological examination, out of total 157 cases, 94 cases were found to be positive for mucormycosis. Of these 94 cases, 63 were males and 31 were females. Age range was from 23 to 75 years. 5 cases showed mixed mucormycosis and aspergillosis infection. Also out of 94 post COVID mucormycosis cases, 72 were diabetic, 21 were hypertensive and 68 had a history of corticosteroid intake for treatment of COVID-19 infection.
Conclusion: Histopathology plays a pivotal role in accurate diagnosis and assessing the severity and invasiveness of mucormycosis. Diabetes mellitus and corticosteroid use are the important associated factors.
Keywords: post COVID -19; mucormycosis; daibetes; steroid therapy
Full Text
Introduction
SARS-COV-2 infection (COVID-19) may be associated with wide range of bacterial and fungal infections [1]. Owing to overuse of immunosuppressants and corticosteroids for treatment of COVID-19 infection, the susceptibility of fungal infection especially mucormycosis has been enhanced. Mucormycos is also known as zygomycosis, is an insidious fungal infection caused by members of mucorales and zygomycotic species [2]. In 1885, Paltauf (the German pathologist), reported the first case of mucormycosis (Mycosis Mucorina) [3]. After infection, they produce lesion of black colour due to which mucormycosis are also known as black fungus [4]. The primary reasons why post COVID-19 patients are more vulnerable for mucormycosis are (a) An ideal environment of low oxygen (hypoxia), (b) High glucose (diabetes, new onset hyperglycemia, steroid-induced hyperglycemia), (c) Acidic medium (metabolic acidosis, diabetic ketoacidosis), (d) High iron levels (increased ferritins), (e) Decreased phagocytic activity of WBC due to immunosuppression (DM/HTN/Steroid) [1].
In diabetic patients, mucormycosis occurs as a destructive and potentially critical condition and ketoacidosis in diabetes accelerate the fungal invasion [5]. Incidence of Rhinocerebral mucormycosis is 33 - 50%. Apophy-somyces elegans is considered as the presumptive aetiological agent [6]. On histopathological examination, the affected tissue with lesions show extensive necrosis with numerous large branching pale-staining, wide, flat non-septal hyphae with branching at right or obtuse angles. Necrotic tissue containing hyphae might be seen with signs of angio – invasion and infarction are seen. Gomori Methamine Silver (Grocott) or Periodic - acid Schiff are the staining of choice.
This study aimed to know the role of histopathology in diagnosis and assessing the prognosis of post COVID-19 mucormycosis cases and to know the predisposing factors.
Material and methods
This is a Prospective observational study conducted at Government Medical College and hospital, Akola over a period of 6 months from April 2021 to September 2021 with ethical committee approval. Functional endoscopic sinus surgery (FESS) and maxillectomy samples from 157 post COVID-19 mucormycosis suspected cases were studied. History of diabetes mellitus, hypertension and corticosteroid therapy was retrieved. All tissue samples were examined under H&E stain and special fungal stain (PAS).
Results
On histopathological examination, out of total 157 cases, 94 cases were found to be positive for mucormycosis. Of these 63 were males and 31 were females. Male to female ratio- 2:1 (Figure 1). Age range was from 23 to 75 years. Mean age was 49yrs. Maximum cases were in age group of 40-50yr i.e 32 (34.04%) (Figure 2). Also out of 94 post COVID mucormycosis cases, 72 (76.6%) were diabetic and 25(26.59%) show concomitant ketoacidosis. 21 (22.34%) were hypertensive. 68 (72.34%) had a history of corticosteroid intake for treatment of COVID-19 infection (Figure 3). Also we found 5 cases showing mixed mucormycosis and aspergillosis infection. The clinical features of cases presented were as shown in figure 4.
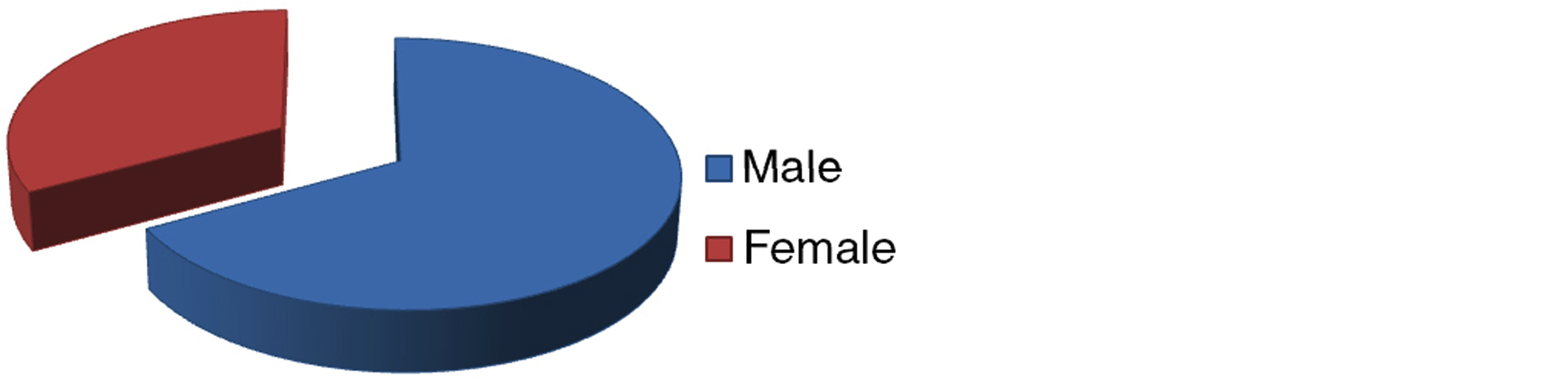
Figure 1: Sex distribution of post COVID-19 mucormycosis cases.
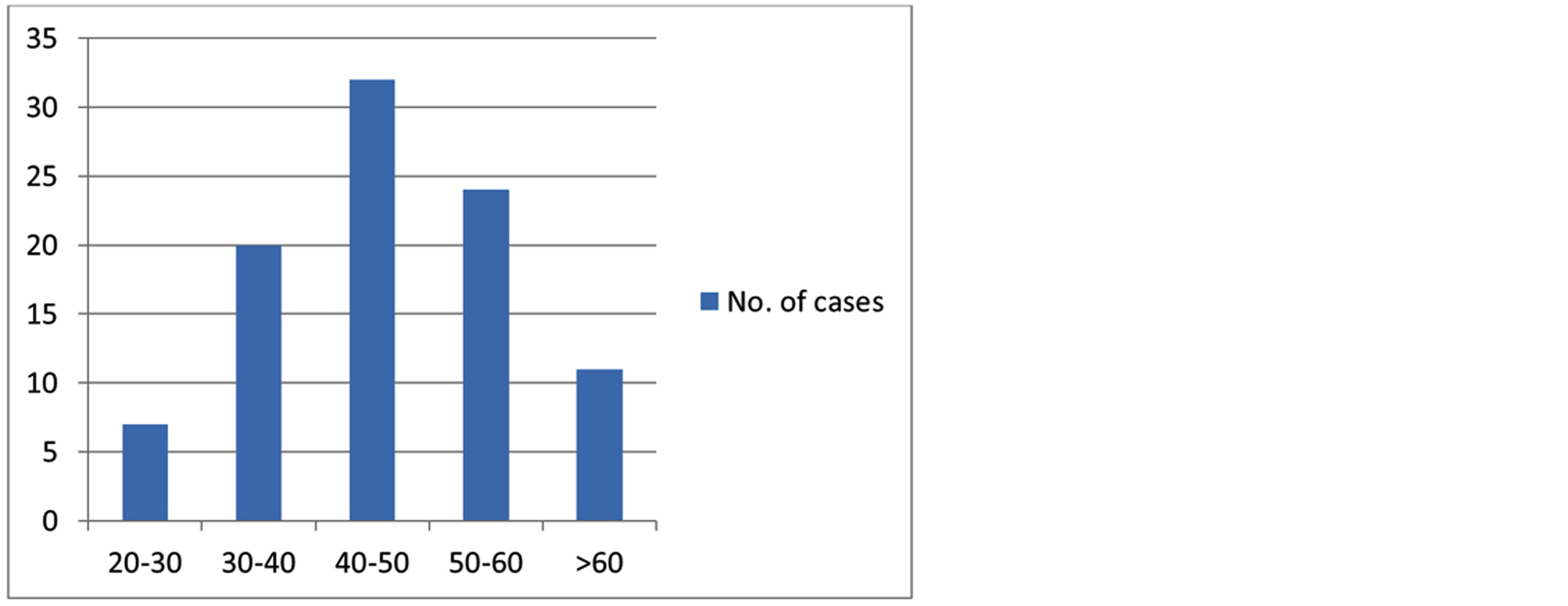
Figure 2: Age distribution of post COVID-19 mucormycosis cases.
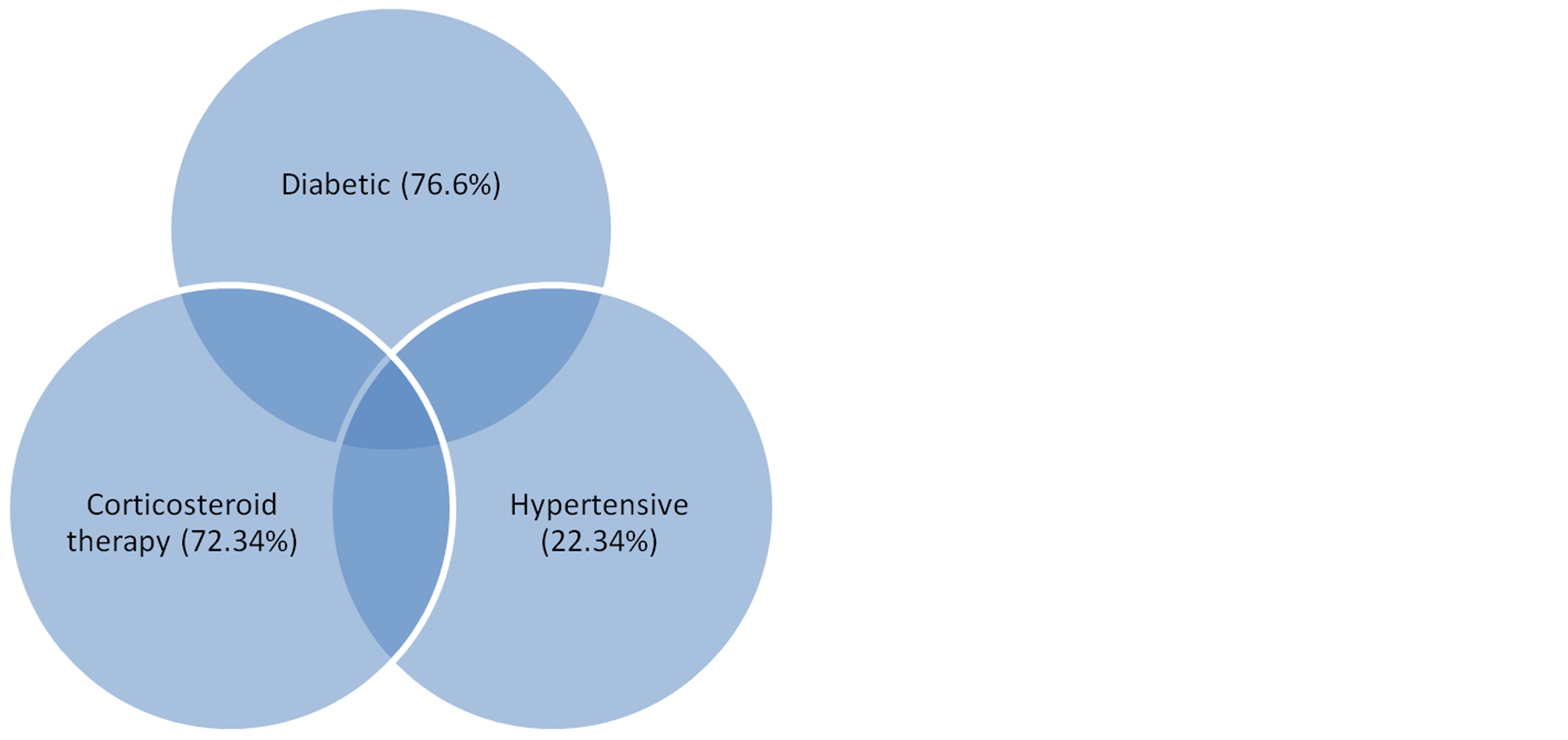
Figure 3: Post COVID-19 mucormycosis cases with overlapping risk factors.
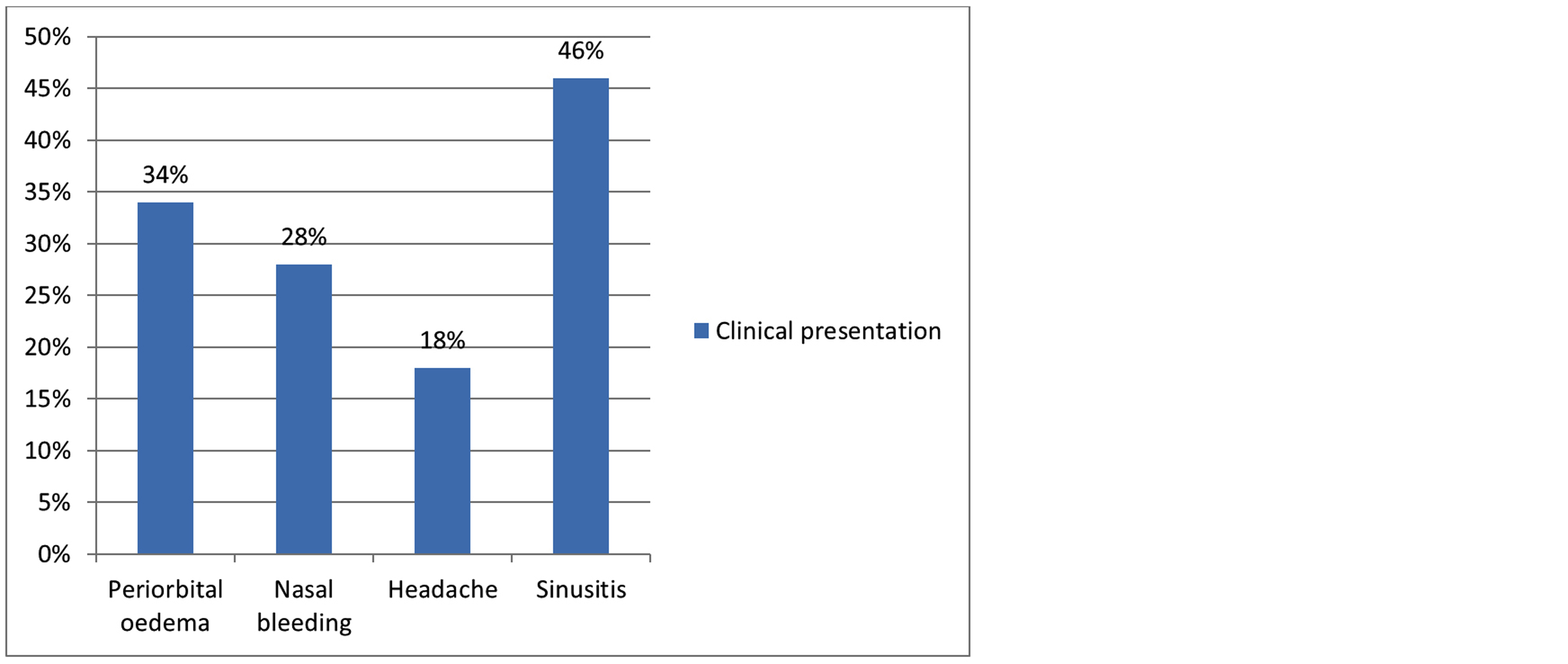
Figure 4: Clinical presentations of patients with post COVID-19 mucormycos.
Histologically on microscopic examination cases with mucormycosis show fungal colonies with short asepted pauci angled hyphaes. Also cases with mixed mucormycosis and aspergillosis infection show fruting bodied and acute angled hyphes of aspergillosis along with hyphes of mucormycosis (Figure 5). Figure 6 shows lactophenol cotton blue stained smear showing sporangia with zygospores of mucor.
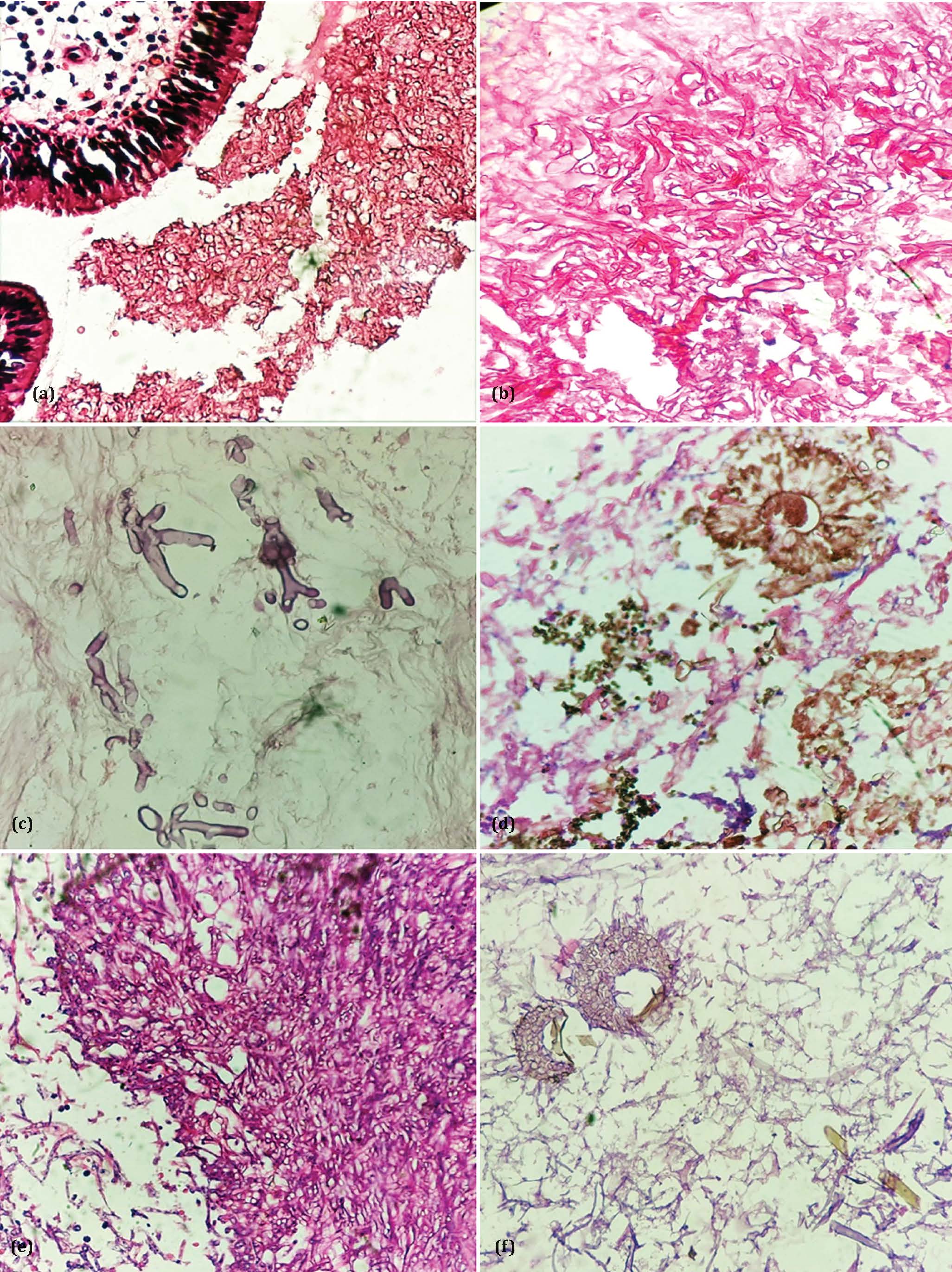
Figure 5: (a) Respiratory mucosa with asepted broad fungal hyphe with right angled branching, (b) Multiple asepted fungal hyphe, (c) Asepted and branched fungal hyphe against necrotic background [40X] H&E, (d) Aspergillosis- Fruiting bodies [40X] H&E, (e) Mucormycosis - fungal ball [40X], PAS, (f) Mixed aspergillus and mucor showing both acute angled branching, septed hyphe, fruting bodies of aspergillus and asepted hyphe of mucor [40X], PAS.
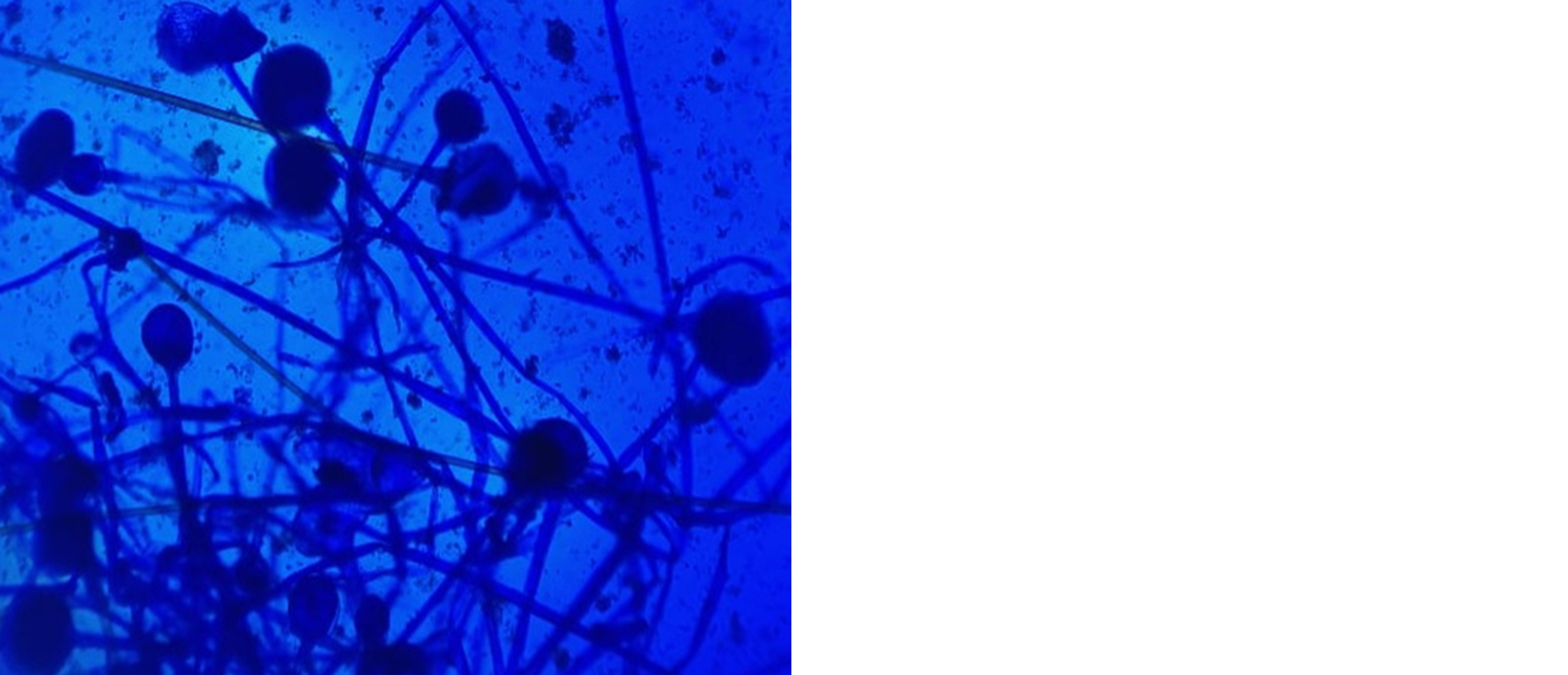
Figure 6: Lactophenol cotton blue stained smear showing sporangia with zygospores.
Discussion
We have found that middle-aged COVID-19 patients who were treated with steroids for diabetes mellitus were more prone to mucormycosis. COVID-19 infection may induce significant and persistent lymphopenia which is a common risk factor for opportunistic infections [7]. SARS-CoV-2 can cause pancreatic injury. Reasons why COVID-19 patients with no history of diabetes have high blood glucose levels [4]. The most common cause of drug-induced hyperglycaemia is steroids [4].
The fungal exposure can be through inhalation, ingestion, direct contact or traumatic inoculation. The clinical hallmark of invasive mucormycosis are necrosis of tissue due to angioinvasion and subsequent thrombosis [8]. Patients commonly present with symptoms of fever, headache, swelling on one side of the face and unilateral periorbital facial pain [9]. Signs seen are nasal or sinus congestion, edema of eyelids and orbital inflammation, internal or external ophthalmoplegia, acute vision loss, black lesions on nasal bridge or upper inside of mouth. Common causes of morbidity and mortality are cavernous sinus thrombosis, disseminated infection and osteomyelitis.
Various laboratory techniques used for detecting Mucor are (a) Direct examination, (b) Histopathological examination (PAS stains, Gomori methenamine, Silver stain), (c) Culture, (d) Molecular methods, (e) Fluorescent in situ hybridization. Gold standard analytic technique for confirmation is the tissue based analysis. The standard protocol for the management is (i) Reversal of risk factors (correction of hypoxia, acidosis, hyperglycemia and electrolyte abnormalities), (ii) Surgical debridement, (iii) Intravenous antifungal medication such as Amphotericin B6, (iv) The mainstay of treatment is systemic Amphotericin B, preferably liposomal preparation [10]. Following a sharp rise in the number COVID-19 patients infected with mucormycosis, the Indian Health Ministry has advised all States to declare mucormycosis itself an epidemic [4].
In present study out of total 157 cases, 94 cases were found to be positive for mucormycosis with male to female ratio- 2:1. Patients were in the age range of 23 to 75 years. Mean age was 49yrs. Maximum cases were in age group of 40-50yr i.e 32 (34.04%). Also in present study, out of total 94 post COVID mucormycosis cases, 72 (76.6%) were diabetic and 25 (26%) show concomitant ketoacidosis. 21 (22.34%) were hypertensive. 68 (72.34%) had a history of corticosteroid intake for treatment of COVID-19 infection. Also we found 5 cases showing mixed mucormycosis and aspergillosis infection. The results of present study was compared with other studies is shown in table 1.
Table 1: Comparison of results of present study with other studies.
|
Parameters
|
Present study
|
Nurani Shaik, etal (2022) [11]
|
Anas M etal (2021) [12]
|
Sree Lakshami etal (2022) [13]
|
|
Male: Female
|
2:1
|
4:1
|
5:1
|
2:1
|
|
Mean age
|
49
|
54
|
56.62
|
51
|
|
Diabetes
|
76.6%
|
80%
|
86.6%
|
81%
|
|
Steroid therapy
|
72.34%
|
36%
|
93.3%
|
-
|
|
Hypertension
|
22.34%
|
-
|
-
|
46%
|
The present study had some limitations as 1) Tertiary centre data do not precisely reflect the disease profile to the community. 2) The present study is based on a limited number of cases and is inadequate to provide conclusive data.
Conclusion
The present study concluded that, SARS-CoV-2 virus along with Diabetes mellitus and steroid therapy forms vicious cycle of hyperglycemia and immunosuppression which leads to severe fungal colonization (Mucormycosis ± Aspergillosis). Histopathology plays a pivotal role in accurate diagnosis and assessing the severity and invasiveness of mucormycosis. Due to association with a very high mortality rate we should put much emphasis on high index of suspicion, early diagnosis, and appropriate management for patient survival. It is essential to assess the risk factors, the types of invasive mycosis to provide appropriate individualized treatment.
Acknowledgement
All our patients and technical staff.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2021; 15:102146,
[2] Suganya R, Malathi N, Karthikeyan V, Janagaraj VD. Mucormycosis: A Brief Review - Journal of Pure and Applied Microbiology. J Pure Appl Microbiol. 2019; 13:161–165.
[3] Mohammadi R, Nazeri M, Sayedayn SMA, Ehteram H. A successful treatment of rhinocerebral mucormycosis due to Rhizopus oryzae. J Res Med Sci Off J Isfahan Univ Med Sci. 2014; 19:72–74.
[4] Rao VUS, Arakeri G, Madikeri G, Shah A, Oeppen RS, et al. COVID-19 associated mucormycosis (CAM) in India: a formidable challenge. Br J Oral Maxillofac Surg. 2021; 59:1095–1098.
[5] Artis WM, Fountain JA, Delcher HK, Jones HE. A mechanism of susceptibility to mucormycosis in diabetic ketoacidosis: transferrin and iron availability. Diabetes. 1982; 31:1109–1114.
[6] Garcia-Covarrubias L, Bartlett R, Barratt DM, Wassermann RJ. Rhino-orbitocerebral mucormycosis attributable to Apophysomyces elegans in an immunocompetent individual: case report and review of the literature. J Trauma. 2001; 50:353–357.
[7] Bhatt K, Agolli A, Patel MH, Garimella R, Devi M, et al. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discoveries. 2021; 9:e126.
[8] Nambiar M, Varma SR, Damdoum M. Post-COVID alliance-mucormycosis, a fatal sequel to the pandemic in India. Saudi J Biol Sci. 2021; 28:6461–6464.
[9] Singh V, Das A, Gupta N, Agarwal AC, Gautam T, et al. Co-infection of mucormycosis and aspergillosis in post COVID-19 patient: A concerning rare case report during second wave of COVID-19 pandemic. IP Int J Med Microbiol Trop Dis. 2021; 7:300–303.
[10] Basile K, Halliday C, Kok J, Chen SCA. Fungal infections other than invasive Aspergillosis in COVID-19 patients. J Fungi. 2022; 8:58.
[11] Shaik N, Bollam A, Konduri G, Sekhar AV. Post-COVID mucormycosis: A retrospective observational study. Indian J Respir Care. 2022; 11:230–233.
[12] Anas M, Choudhary RK, Alam N. Clinical profile and risk factors associated in patients of mucormycosis in COVID-19 pandemic: A study in a tertiary centre. Int J Res Med Sci. 2021; 9:2780–2786.
[13] Lakshmi IS, B. Kumari S, Jyothi CH, Devojee M, Malini KP, et al. Histopathological Study of Mucormycosis in Post COVID-19 patients and factors affecting it in a tertiary care hospital. Int J Surg Pathol. 2023; 31:56–63.