Full Text
Introduction
Angular deformities of the knee, a common problem in the early years of life are frequently encountered in paediatric orthopaedics not only because of very high incidence of these deformities but also because of major parental concern in the present highly demanding sports oriented society [1].
For the majority of children, the problem represents a normal physiologic variation, correcting spontaneously which may often require only expectant management, benign neglect and parental reassurance. In contrast to physiological deformities, pathological deformities aggravate as the underlying disease progresses and also with skeletal growth with age maturity [2].
Appropriate medical management of conditions such as rickets, osteogenesis imperfecta, and neuromuscular conditions is paramount to achieving good outcome but may not prevent the need for surgical realignment of the lower limbs [3].
The concept and the method of physeal growth arrest, after first time introduced by Dallas Phemister in 1933, variety of modes of surgical ablation of hemiepiphysis and different types of implants for the same have been developed and analysed from time to time [1]. Even though the surgical ablation has remained the prototypic form of asymmetrical physeal suppression, unpredictable growth of the remaining physis in some patients renders overcorrection or undercorrection inevitable [1, 3].
Hemi-epiphysodesis using 8-plate is a well accepted method of correction for many deformities in all age children with any diagnosis due to its tension band technique and less complications in comparison to staples. 8-plate technique has rapidly gained popularity and, studies show encouraging results. The 8-plate is purported to allow guided growth with the prospect of reducing the complications related to physeal stapling, and also providing more rapid correction than stapling [4-6].
Because of the logic, simplicity and versatility with flat learning curve associated with 8-plate technique. This technique has rapidly gained popularity, but there is scant literature with regard to its effectiveness especially in sub- continent.
The objectives of study were to assess the correction of angular deformities of knee in children using guided growth technique 8 plates, and to assess the time of correction, rate of correction and duration of time taken for correction of the angular deformity of knee in children using guided growth technique.
Materials and methods
This is a study conducted on pediatric orthopedic patients over a period of 4 years from June 2018 to June 2022, with angular deformities of knee presented to Sparsha Hospital, Bangalore, Karnataka, India. 25 children were included in the study with total 45 knees having varus or valgus angular deformities, of which 20 were bilateral and 5 were unilateral.
Child with angular deformities around knee (varus / valgus) surgically treated by eight plate application were included in the study. Patients with less than 12 months of predicted growth remaining, physiologic deformity and muscular dystrophy were excluded in the study.
The information collected regarding all the selected cases were recorded in a Master Chart. Data analysis was done with the help of computer using Epidemiological Information Package (EPI 2010) developed by CDC, Atlanta. Using this software range, frequencies, percentages, means, standard deviations, chi square and 'p' values were calculated. Kruskal’s Wallis chi-square test was used to test the significance of difference between quantitative variables [4].
All the patients were symptomatic and were followed for the next minimum 12 months for any progression or regression of the deformity. After following for the minimum 12 months, those children without any spontaneous improvement noted after observation were selected for the present study. If the mechanical axis was falling outside the 3+ or 3- stevens zone, another criterion was followed. Patient’s detailed clinical history was sought from the parents, the age at presentation; gender and side involved were noted in the proforma. The nature of symptomatic deformity, its origin, duration and progression or regression was noted.
All the surgeries were performed under general anaesthesia in supine position, tourniquet was applied to limb to be operated. Limb painted and draped. Under tourniquet control, each incision was placed over mid-sagittal plane centred on the physis 2–3-cm long, on the medial aspect in case of genu valgum and on the lateral aspect in case of genu varum under fluoroscopic guidance.
Deep fascia was incised along the line of skin incision. Soft tissue dissected and subfascial plane created without damaging periosteum. A needle was inserted through the perichondrial ring to localise the physis (confirmed fluoroscopically). The appropriate size of the eight-plate was applied over needle. The study was showed mean pre-operative deformity genu varum was 28.8 degrees and 8.4 degrees of genu valgum (Tables 1 and 2).
Table 1: Amount of correction of Genu valgum.
|
Genu valgum
|
Pre-op tibiofemoral angles (degrees)
|
Post-op tibiofemoral angles (degrees)
|
p value
|
|
No. of knees
|
38
|
38
|
< 0.0001
Significant
|
|
Mean
|
19.79
|
6.05
|
|
SD
|
4.56
|
1.73
|
Table 2: Amount of correction of Genu varum.
|
Genu varum
|
Pre-op tibiofemoral angles (degrees)
|
Post-op tibiofemoral angles (degrees)
|
p value
|
|
No. of knees
|
7
|
7
|
0.091
Not significant
|
|
Mean
|
17.29
|
9.17
|
|
SD
|
5.85
|
4.45
|
Out of 45 knees studied, implant removal was done in 19 cases at a total mean duration of 14.15 months with 17 cases of idiopathic group (mean removal of 14.41) and 2 cases of pathological group (mean removal of 12 months) (Table 3).
Table 3: Mean duration of implant removal.
|
|
Implant removal done
|
Total
|
Total mean duration of
Implant removal
|
|
Idiopathic group
|
Pathological
group
|
|
No. of knees
|
17
|
2
|
19
|
14.15 months
|
|
Mean duration of removal
|
14.41 months
|
12 months
|
|
We used one plate per physis, because it serves as a tension band. The position of the plate is confirmed under anteroposterior and lateral views of fluoroscopy. Threaded guide pins are inserted through the centres of holes in the plate (Figure 1). The direction of the guide pins are such that they do not encroach on the physis when the screws are finally seated. Starting hole is drilled 3.2-mm through the cortex. The cannulated 4.5-mm self-tapping screws are applied with appropriate length (16/24/32 mm) chosen (Figure 2).
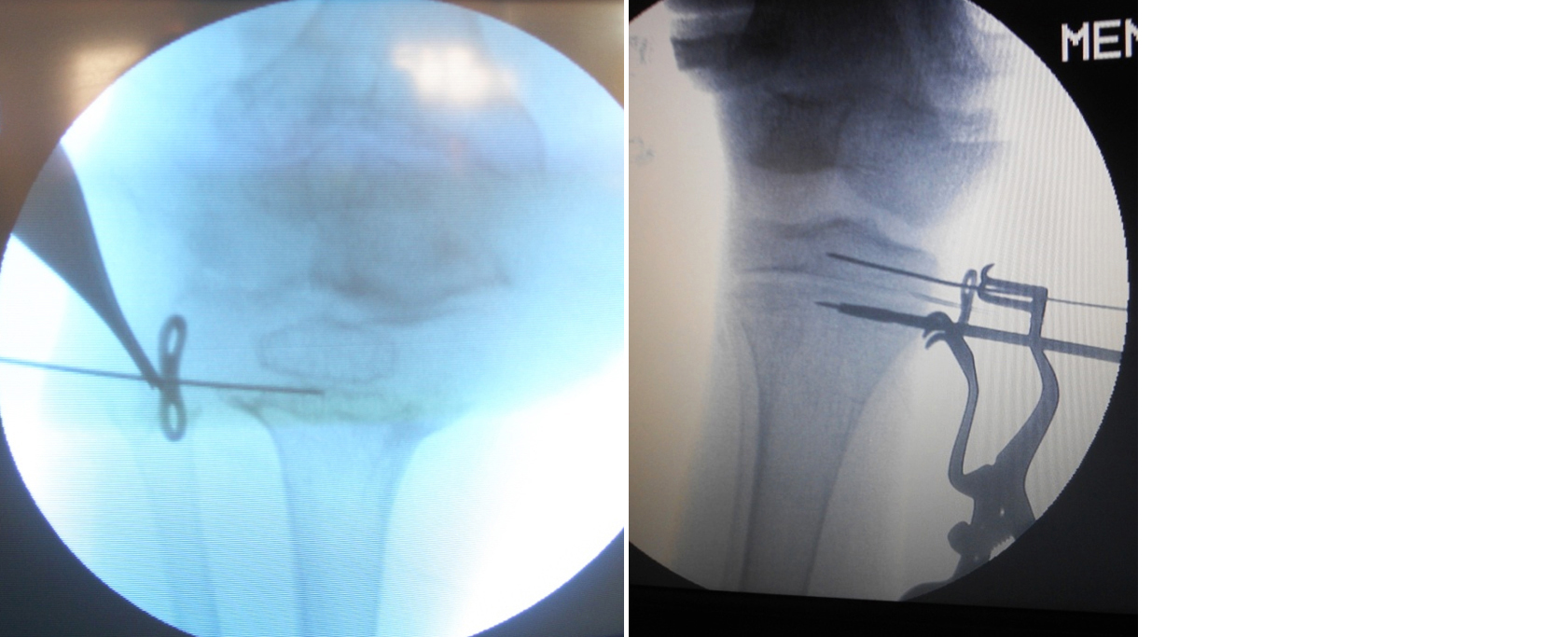
Figure 1: (a) Insertion of physeal K-wire, (b) Guide wires over 8-plate.
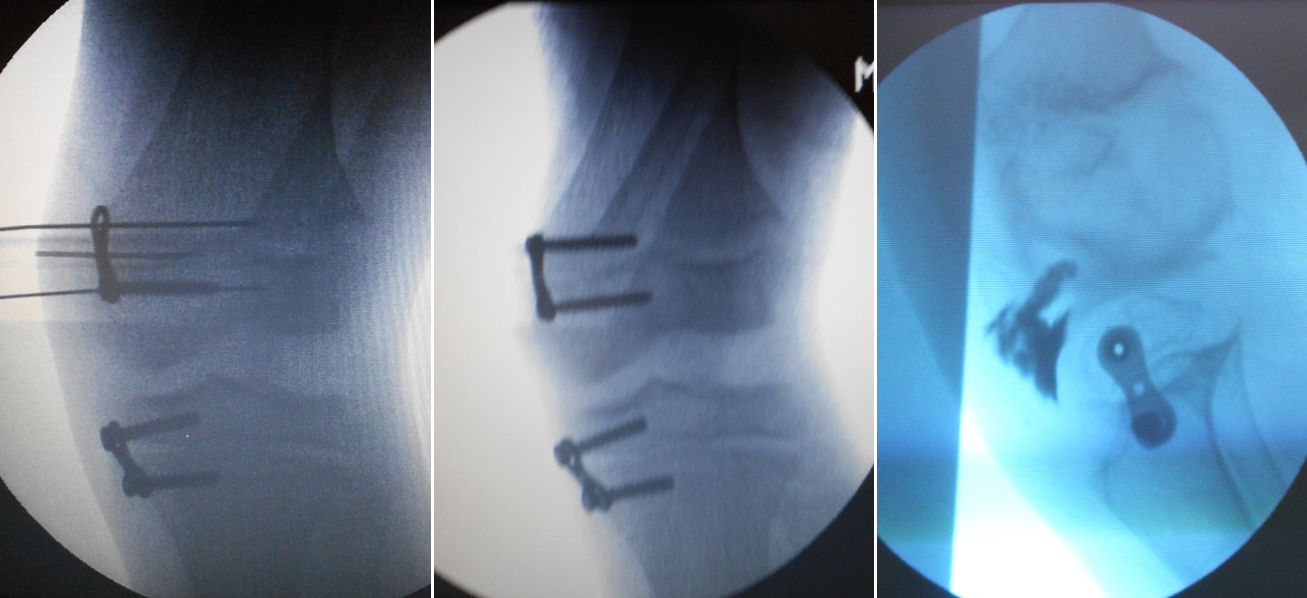
Figure 2: (a) 8-plate screw fixation, (b) AP, and (c) Lateral views.
Upon removal of the guide pins, each screw is rechecked and securely tightened to Wound is closed in layers and a compression bandage is applied without any immoblisation. Immediate motion and weight-bearing was started, with crutches as needed for comfort.
Post-operative protocol
The patient is started with activities as tolerated and or those children who are slow to mobilise, physical therapy is started. Periodic follow-up at 3-month intervals was done as documented for deformity correction. At each follow up full length anteroposterior scanograms were performed and assessed for the mechanical axis, tibiofemoral angles, mechanical lateral distal femoral and medial proximal tibial angles. Any changes in the deformity including recurrence, overcorrection, rebound growth, limb length discrepancies or saggital plane deformities were documented. Upon the correction of the deformities with neutralisation of the mechanical axis, and plate removal was scheduled accordingly. Patients were continued on at least an annual basis, to watch for rebound growth, limb length discrepancy, or premature physeal closure.
Discussion
In our series, we studied cases from 3 to 13 years of age; the mean age was 6.48 years with 84% predominating up to age of ten years. 13 (52 %) were boys and 12 (48 %) were girls. Out of 25 cases, twenty cases (80%) were bilateral and five, unilateral. Our age group was comparable to study by Burghardt et al [7] who had 43 patients with age group ranging from 4-14 years, mean age of 9.7 years and similar to Stevens et al [4] study of 34 patients with age group ranging from 1.7-17.5 years and a mean of 10.5 years of which 20 were bilateral and rest unilateral. Average age is less in our study since 81 % of cases belong to age group of up to 10 years where as in Ballal et al [8] and Das et al [9] the number of children around 10 years or more was predominant. This is because major number (64%) of deformities was idiopathic in nature which was presented in early years of childhood.
In current series, 21 cases had genu valgum and 5 cases genu varum. Out of 21 (84%) cases of genu valgum knees, 1 had thalassemia, 1 had hypophosphatemic rickets and rest were idiopathic. Of the 5 (16%) genu varum cases, 1 had spondyloepiphyseal dysplasia, 1 had pseudoachondroplasia and 2 had hypophosphatemic rickets.
Our study was comparable to Burghardt et al [7] which had 39 patients with genu valgum and 4 genu varum and Boero et al study where out of 58 patients, 45 were genu valgum and 12 genu varum where as in Das et al [9] had 36 genu varum, 14 genu valgum and 4 wind swept deformities.
The length of final follow up in our study was 27.84 months ranging from 14 to 40 months. The mean follow up of Stevens et al [4] was 14 to 26 months, Ballal et al [8] was 12.4 months ranging from 6 to 32 months, Burghardt et al [7] was 9.5 months, Wiemann et al [10] and Das et al [9] mean follow up was 38 months.
Out of 45 deformities, 38 knees had mechanical axis in zone plus 3 of Stevens’s zones, five knees had mechanical axis passing through minus 3 zone, one knee in minus 2 zone and one in minus 1 zone. Although most of studies done after Stevens et al [4] mention about the mechanical axis deviation, no exact data is available on how many patients at the time of presentation had deviation of mechanical axis and at final outcome except for the Burghardt et al [7].
In the current series, the segmental mechanical parameters for the deformity as measured by mechanical lateral distal femoral angle and mechanical medial proximal tibial angle were significantly associated with surgical outcome, suggestive of the differential growth alteration at the distal femoral and proximal tibial physes which contributing to deformity correction individually at the level of knee.
In our study, the mean medial proximal tibial angle in this study was 95.49 degrees at the starting which was corrected to 88.18 degrees after the surgery which was similar to Burghardt et al [7] which had mean pre-operative of 94 degrees which got corrected to 87 degrees. The mean lateral distal femoral angle in was 85.11 degrees at the starting which was corrected to 88.68 degrees after the surgery which was similar to Burghardt et al [7] which had mean pre-operative of 82 degrees which got corrected to 91 degrees.
In our study the mean preoperative deformity (tibiofemoral angle) ranged from 9 degrees of genu varum to 35 degrees of genu valgum. The mean preoperative genu valgum deformity was 19.79 degrees with range from 13-35 degrees and genu varum deformity was 17.29 degrees (9-25 degreees) which was comparable with study by Stevens et al [4] in which case preoperative deformity range from 7 degrees to 30 degrees and similar to study by Schroerlucke et al [6] with preoperative varus 14.6 degrees and valgus 17.2 degrees. Our study was similar to Ballal et al [8] in which mean pre-operative deformity genu varum was 28.8 degrees and 8.4 degrees of genu valgum.
We had total four cases with complications. 2 knees in a case of bilateral genu varum remained persistently varus at the final follow up period of 24 months which was a case of sick physis secondary to pseudoachondroplasia. One case of bilateral genu varum secondary to hypophosphataemic rickets which had overcorrection of deformity and drifted in to genu valgum on one side after removal of plates and one case of bilateral idiopathic genu valgum which had rebound deformity after full correction and plate removal at the final follow up period of 24 months in one of the knees of which was re-operated and plates were reapplied for the correction. None had complications related to wound, hardware failure or iatrogenic sagittal or limb length discrepancies.
Our study was comparable to Stevens et al [4] in which four patients (11.7%) with adolescent genu valgum who underwent guided growth at or younger than 11 years have experienced bilateral rebound growth and recurrent deformity in 8 femora after plate removal. The mean time to recurrence was approximately 14 months after plate removal; each electively underwent repeat guided growth with plates. One of the 2 recalcitrant Blount patients case underwent revision of fixation. One patient had wound related complications which resolved with oral antibiotics. In study from Ballal et al [8] showed 3 complications in which there was one migration, one deep infection and a case of one rebound deformity.
In our series, 91.1% of the deformed knees were corrected fully at the mean final follow up period of 27 months, neutralizing the mechanical axis and correction of the deformity which is comparable to study by Burghardt et al [7] with a success rate of 91% at mean follow up of 9.5 months. Our study was similar to study by Weimann et al [10] with a success rate of 87.5 %.
Some of the most severe deformities (3 patients) found in the pathological group did not achieve full correction, but as stated by Schroerlucke et al [6], in such cases, even partial correction is a positive result. We believe even the small correction achieved will subsequently make osteotomies technically easier.
We agree Ballal et al [8] and Levine et al [5] who proposed that after the age of 8, an angular deformity of less than 10o can be considered cosmetic and does not warrant surgery. However, surgical intervention should be considered for a deformity greater than 10° with a predicted remaining time for growth of at least 12 months.
Out of 45 knees studied, implant removal was done in 19 cases at a total mean duration of 14.15 months with 17 cases of idiopathic group (mean removal of 14.41) and 2 cases of pathological group (mean removal of 12 months). It was comparable to Boero et al [11] where average implant removal was 14 months with 11 months idiopathic group and 18 months in pathological group.
We observed that the rate of correction was slower in the pathological group than in the idiopathic group. The degree per month of correction was also slower in the pathological group than in the idiopathic group. This, in all likelihood, is a reflection of physeal compromise that is characteristic of dysplasias and endocrinopathies [12].
No hardware failure was observed in this study. This information is consistent with three other studies but differs from the data from one study. Perhaps patient selection and attention to technical details would explain the difference. We did not experience long-term problems with the positioning of screws after implantation. However, there is a need to research newer design of implants to correct the torsional deformities of long bone [13] and correction of limb length discrepancies [14]. In this preliminary study of outcomes in Indian patients, improvements were found in all patients except one case following guided growth to correct angular deformities using eight-plate.
The limitations of the study included the small number of patients and the short duration of follow up with an average of 48 months.
Conclusion
8-plate is technically simple and potent tool to correct genu valgum and varus deformities around knee in children without need for osteotomies in many children. We consider the eight-Plate the best solution for the treatment of pediatric angular deformities, be they idiopathic or due to an underlying pathological condition. Rebound deformity, although uncommon and unpredictable, can safely be managed by repeated guided growth with the eight-plate. Medical management along with hemiepiphysiodesis using growth plate gives good out come in case of metabolic conditions like rickets. Based on the low complication rate, patient acceptance, and the rapidity of improvement, this technique may be used as treatment of choice.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Phemister DB. Operative arrestment of longitudinal growth of bones in the treatment of deformities. J Bone Joint Surg Am. 1933; 15:1–15.
[2] Blount WP, Clark GR. Control of bone growth by epiphyseal stapling. J Bone Joint Surg. 1949; 31A:464–471.
[3] Blount WP. A mature look at epiphyseal stapling. Clin Orthop Relat Res. 1971; 77:158–163.
[4] Stevens PM, MacWilliams B, Mohr RA. Gait analysis of stapling for genu valgum. J Pediatr Orthop. 2004; 24:70–74.
[5] Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982; 64:1158–1163.
[6] Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FA. Failure of orthofix eight-plate for the treatment of blount disease. J Pediatr Orthop. 2009; 29:57–60.
[7] Burghardt RD, Specht SC, Herzenberg JE. Mechanical failures of eight-plate guided growth system for temporary hemiepiphysiodesis. J Pediatr Orthop. 2010; 30:594–597.
[8] Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br. 2010; 92:273–276.
[9] Das SP, Pradhan S, Sahoo PK, Mohanty RN, Das SK. Our experience with correction of angular deformities of knee by flexible figure of 8-plate hemiepiphysiodesis. IJPMR. 2012; 23: 68–73.
[10] Wiemann JM, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009; 29:481–485.
[11] Boero S, Michelis MB, Riganti S. Use of the eight-Plate for angular correction of knee deformities due to idiopathic and pathologic physis: initiating treatment according to etiology. J Child Orthop. 2011; 5:209–216.
[12] Feng WJ, Dai ZZ, Xiong QG, Wu ZK. Temporary hemiepiphysiodesis using eight-plates for angular deformities of the lower extremities in children with X-linked hypophosphataemic rickets. Int Orthop. 2023; 47:763–771.
[13] Abood AA, Hellfritzsch MB, Møller-Madsen B, Brüel A, Westersø TS, et al. Controlled rotation of long bones by guided growth: A proof of concept study of a novel plate in cadavers. J Orthop Res. 2022; 40:1075–1082.
[14] Tolk JJ, Merchant R, Calder PR, Hashemi-Nejad A, Eastwood DM. Tensionband Plating for Leg-length Discrepancy Correction. Strategies Trauma Limb Reconstr. 2022; 17:19–25.