Full Text
Introduction
Zoonoses have been defined as diseases and infections that are naturally transmitted between vertebrate animals and humans. Although Echinococcosis has a benign presentation, it is a serious disease and should always be included in the differential diagnosis of any mass lesions occurring in the lungs. There are four species within the genus Echinococcus, with E. granulosus and E.multilocularis being the most common, causing cystic echinococcosis (CE) and alveolar echinococcosis (AE) [1]. The clinical presentation of the disease is non-specific. It commonly involves the liver, lungs, brain and adrenal glands The lung is the second most common site of involvement with Echinococcus granulosus in adults after the liver (10-30% of cases), and the most common site in children [2]. The life cycle of Echinococcus includes a definitive host (usually dogs) and an intermediate host (such as sheep, goats or swine). Humans are incidental hosts and represent usually the dead end for the parasite [3]. The lung is involved in 2 forms of human hydatidosis caused by the cystic larval stage of the tapeworm, Echinococcus. Cystic hydatid disease is caused by Echinococcus granulosus and alveolar hydatid disease by Echinococcus multilocularis. Pulmonary hydatid cysts are characteristically solitary and three- fourths of patient’s cysts are in one lobe, more often lower lobes, posterior more than anterior and more common on the right [4, 5].
Our patient was having a unilateral hydatid cyst. Cough and chest pain are the commonest symptoms, and clinical signs are rarely definitive except for an occasional fluid thrill in very large cysts [4]. Radiology remains the mainstay of diagnosis, being 98-100% accurate in most cases. Hydatid cyst cases superinfected with pyogenic organisms have been reported previously.
Brucellosis is a common zoonotic infection with multisystem involvement caused by Brucella species. Transmission of it to humans occurs mainly through the consumption of infected, unpasteurized animal milk and milk products [6]. Treatment options include doxycycline 100 mg twice a day for 45 days, plus streptomycin 1g daily for 15 days. The main alternative therapy is doxycycline at 100 mg, twice a day for 45 days, plus rifampicin at 15mg/kg/day (600-900mg) for 45 days [6]. Here, we present a case of hydatid cyst disease along with Brucella and review the literature on other hydatid cyst cases in association with pyogenic organisms in an immunocompromised patient. We discuss the coexistence of brucellosis and lung hydatid echinococcosis in immunocompromised (HIV+) adult patient. We hypothesize that the coexistence of both entities is infrequent but may occur due to increased and uncontrolled incidence of the diseases [7].
Surgery is the treatment of choice for pulmonary hydatid cysts and medical treatment is beneficial in cases which are inoperable or when patients do not consent for surgery. Albendazole is recommended at doses of 10-15 mg/kg/day for 4 weeks separated by 14-day intervals for 2 or more courses. However protease inhibitors and benzimidazoles interfere strongly at the CYP3A4-level. Hence very low doses of albendazole/ mebendazole achieve sufficient therapeutic levels in HIV patients taking protease inhibitors [4].
Thus pulmonary hydatid cysts can present as pulmonary infiltrates especially with secondary infection, in Indian patients more so in those with AIDS. This case highlights the importance of clinico-radiological correlation in medical diagnosis.
Case presentation
A 47-years-old male patient came for his usual followup and complained of high grade intermittent fever and chills since 5 days, cough, generalized myalgia, headache and was detected with retroviral disease since 21 years and had a history of pulmonary hydatid cyst which was settled with surgical intervention. He was an ex-military officer and now works in his agricultural land. Clinical examination revealed an averagely built and nourished man with normal vital parameters and a respiratory rate of 20 bpm. He was admitted in the hospital and required investigations showed moderate thrombocytopenia, dengue IgM and parasite F/V were sent and found to be negative and his absolute CD4 count was found to be 262 cells/microlitre. The patient started on intravenous cefoperazone sulbactum a broad spectrum antibiotic to cover both gram positive and gram negative bacteria. With due course the patient improved symptomatically and was discharged. After a couple of months he presented to the hospital with intermittent high grade fever-past 4 months, loss of appetite, generalized weakness, weight loss- 2 kgs, dryness in mouth, right upper chest swelling since a week and on examination temperature was 101F, respiratory rate of 18/min. There were scattered crackles unilaterally and reduced breath sounds with increased vocal resonance in the right upper lobe. Chest swelling was oval in shape, soft in consistency, no skin infiltration with mobile on parallel plane and immobile on vertical plane which is probably arising from below the muscle plane. Outside blood count revealed increased CRP levels (11.41mg/dl) and absolute CD4 count was found to be 326 cells/microlitre. Sputum AFB was negative, sputum gram stain showed scanty pus cells, plenty epithelial cells and plenty gram positive cocci in pairs and occasional gram negative bacilli were seen, sputum culture and sensitivity showed growth of normal flora no other pathogens could be isolated, GENE-XPERT- MTB not detected. Chest x-ray was done and showed pleural based lesion and with reticulonodular opacities (Figure 1).

Figure 1: Chest x-ray PA (A well-defined homogeneous radiopaque lesion with broad based towards the costal pleura noted in the right upper and mid zones - likely represents pleural based lesion, focal cortical destruction along the inferior surface of right 3rd and 4th ribs. reticulonodular opacities noted in right lower zone).
A CT scan of chest, revealed a large fairly well-defined pleural based complex cystic lesion showing multiple internal septations and daughter cysts in the right pleural cavity in the upper and mid zones along the anterolateral chest wall measuring approximately 10.7×8.4×10.5 cm. The lesion is infiltrating the chest wall muscles with encasement of the lateral and anterior aspects of the right third rib which show ill-defined permeative lytic lesions. Mild scalloping of the right fourth rib was seen. No evidence of any calcifications. Compression atelectasis of the adjacent lung parenchyma was seen. It extends into the right axilla and involves the pectoralis minor muscle. Minimal peripheral enhancement was seen in the superoanterior aspect of the lesion and in the chest wall. Small pleural based non-enhancing cystic lesion measured 14×10 mm adjacent to the posterior segment of the right lobe with focal extra pleural extension. Varicose and cystic bronchiectatic changes with surrounding fibrotic lesions were seen in the anterior basal segment of the right lower lobe and in the medial segment of the right middle lobe. Paraseptal emphysematous changes in the basal segment of the right lower lobe were seen (Figure 2).
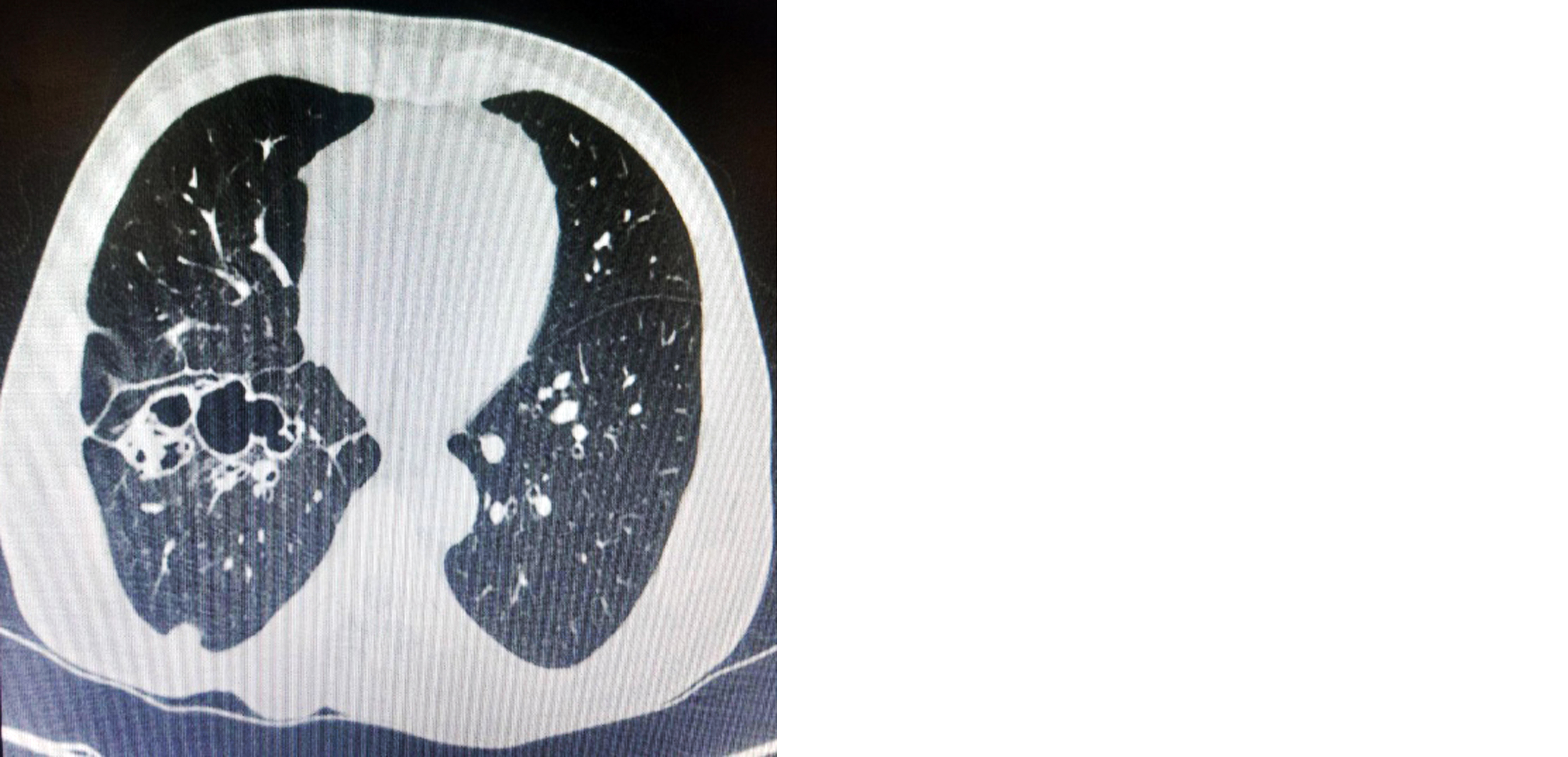
Figure 2: Computed tomography chest - Paraseptal emphysematous changes in the basal segment of the right lower lobe.
Cardiothoracic vascular surgeon opinion was taken for surgical intervention but due to proximal ulnar osteotomy (PUO) surgery got withheld and was discharged with followup. On review positron emission tomography (PET) CT Whole body did not reveal any hydatid cysts in the liver and other organs. Inconsideration of PUO and severe myalgia routine viral tests and sputum culture tests and PET CT were done and came out to be negative except brucella IgG(93.91) and IgM(26.19) antibodies which were significantly positive suggestive of brucellosis.
According to BMC Infectious Diseases, among the 35 patients, 19 patients (54.29%) were hospitalized with the characteristic of PUO, and the misdiagnosis rate was 100% [8], and of course false positive antibodies rate is significant in diagnosis of brucella but with appropriate brucellosis treatment i.e., oral doxycycline 100mg twice daily, rifampicin 450 mg once daily, the patient's response has been positive, and the current medical approach for the hydatid cyst i.e., oral albendazole 400mg twice daily, is being closely. Overall, the patient's condition is stable, and the medical interventions have been successful in managing the patient's symptoms effectively, regular follow-up appointments as an outpatient have been maintained.
Discussion
Pulmonary hydatid cysts are treated by pharmacotherapy and/or surgery. Surgical intervention is the treatment of choice though pharmacotherapy may also be useful in selected patients. Medical therapy of pulmonary hydatid cyst includes a benzimidazole group of drugs, for example, mebendazole (MBZ) or albendazole (ABZ). ABZ is preferred, as it has better bioavailability, can be used with lower doses and is more effective [9].
After diagnosing it as a pulmonary hydatid cyst with the help of CT chest, our patient was started on benzimidazolesi. Albendazole 400mg twice daily and other medicine for symptomatic relief. The usual recommended dosage of ABZ is 10–15 mg/kg/day, taken twice daily. The optimal duration of pharmacotherapy in pulmonary hydatidosis is not known, but it should be given for a minimum period of 3–6 months.
In the past, the drug was given in several one month courses interrupted by 14-day intervals. However, studies shows that continuous therapy is more efficacious, as it achieves higher drug levels on a sustained basis and higher penetration into the parasitic mass. Benzimidazoles act by inhibiting microtubular assembly within the parasite, leading to impaired glucose absorption through the wall of the germinative cell layer of the larva. It results in glycogen depletion and degeneration of the endoplasmic reticulum and mitochondria of the parasite, along with an increase in lysosomes and subsequent autolysis of cells [9].
Treatment options for brucellosis include doxycycline 100mg twice a day for 45 days, plus streptomycin 1g daily for 15 days. But because of its unavailability in oral form and its possible occurrence of nephrotoxicity streptomycin was not advised in this patient. The main alternative therapy is doxycycline at 100mg, twice a day for 45 days, plus rifampicin at 15mg/kg/day (600-900mg) for 45 days [6]. This patient was started on oral doxycycline 100mg twice daily along with oral rifampicin 450 once daily.
Although surgery is the mainstay of treatment for hydatid cyst, in this patient we opted for pharmacotherapy because he was having active high grade fever during which surgical intervention was not advised and was stated on albendazole 400 mg OD for 28 days.
Conclusion
A high degree of clinical suspicion combined with history and clinical examination supported by laboratory investigations are required for the diagnosis of both pulmonary hydatid cyst and brucellosis because of its varied symptomatology. This case presents the importance of considering brucellosis and hydatid cyst as a differential diagnosis in patients who are immunocompromised and manifesting the symptoms.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Sekar N, Shah NK, Abbas SS, Kakkar M. Roadmap to combat zoonoses in India initiative. Research options for controlling zoonotic disease in India, 2010-2015. PLoS One. 2011; 6:e17120.
[2] Dudha M, Shaikh Z, Bhaiyat M, Wadiwala IJ, Bhaiyat ZT. A case of echinococcal cyst of the lung. Respir Med Case Rep. 2018; 25:286–292.
[3] Sarguna P, Bilolikar AK, Rao A, Mathur DR. Brucellosis in association with hiv infection- A case report, Indian J Med Microb. 2002; 20:221–222.
[4] Shenoy VV, Joshi SR, Aklujkar AP, Kotwal VS, Nadkarni NA, et al. Pulmonary hydatid cyst in HIV-1 disease. J Assoc Physicians India. 2005; 53:1070–1072.
[5] Lahiri K. Parasitic infections of the respiratory tract (diagnosis and management). J Postgrad Med. 1993; 39:144.
[6] Brucellosis. Available from https://www.who.int/news-room/fact-sheets/detail/brucellosis.
[7] Niknejad M, Khoshnaw K, Yap J. Pulmonary hydatid infection. Available from: https://radiopaedia.org/articles/pulmonary-hydatid-infection?case_id=hydatid-cyst-lung
[8] Wu Z, Song Z, Wang W, Xi W, Jin D, et al. Human brucellosis and fever of unknown origin. BMC Infect Dis. 2022; 22:868.
[9] Sarkar M, Pathania R, Jhobta A, Thakur BR, Chopra R. Cystic pulmonary hydatidosis. Lung India. 2016; 33:179–191.