Full Text
Introduction
Population aging is transforming the world which mainly include demographic and epidemiological transition, in which non-communicable chronic diseases are becoming the major cause of death as well as contributors of major diseases and disability. Global aging will affect economic growth of the nation as well [1]. Elderly people are the most rapidly growing population group worldwide and as per census 2011, persons age 60 years or above are nearly 104 million in India [2]. Despite this large number in India, geriatric care facilities has yet not received attention it deserves [3]. To provide the health care needs of this growing numbers of the vulnerable heterogeneous population, reliable data are still lacking and with recognition of the need the present study has been designed [3].
Geriatric patients require more complex evaluations, more consultations with other specialists, and a higher percentage of readmissions. In young patients who are admitted to an emergency department, have certain clinical factors with the acute disease which surely influence the outcome. However, this is not the case in the elderly patients, where the resolution does not derive from the attention of a single cause. In elderly, the severity of the acute disease and its prognosis are affected by the functional, emotional and cognitive states, the level of comorbidity, the degree of polypharmacy and the social support networks. The lack of knowledge of the elements in the elderly patients in emergency care ultimately results in diagnostic errors and more serious therapeutic errors and ultimately prognosis.
A country like India is experiencing quadruple burden of disease which are chronic non-communicable diseases, human immunodeficiency virus (HIV) infection/ acquired immunodeficiency syndrome (AIDS), poverty related conditions and trauma. However, among the elderly, non-communicable or chronic diseases are the main contributors to the burden of disease worldwide. Over the past few decades, in developed countries, geriatric health services are having a great advancement but India is still behind and that has resulted in the lack of epidemiological data on aging and associated burden of diseases [4].
The present study was conducted with the aim to study clinical profile of geriatric patients admitted at Civil Hospital, Ahmedabad with objectives to study various clinical presentation of elderly patients of age ≥65 years, to study medical complications and the co-morbid conditions in the same.
Materials and methods
It was a prospective observational study which was conducted after the permission from the institutional ethical committee at the Department of Medicine, Civil Hospital, Ahmedabad for the duration of 2 years from August 2019 to July 2021. Patient ≥65 years of age, who had acute emergency illness and admitted in the hospital were included in the study, while patients less than 65 years of age, patients with history of fall, trauma and acute poisoning and patients and/or patient’s relatives who had not given consent for the study were excluded from the study.
Total 100 patients, who has fulfilled the inclusion criteria were enrolled in the study. Detailed history taking and clinical examination was done as per prescribed proforma and all essential radiological and biochemistry investigation done as per requirement. All the collected data has been entered in Microsoft Excel sheet. Results were presented as mean ± standard deviation (SD) or percentages. Continuous variables were analysed for normalization and compared using the student t test. Inter group comparisons were made using chi-square test. A cut-off value of p<0.05 was considered statistically significant. All patients were given treatment as per standard treatment protocol.
Results
Among 100 patients, 55 (55%) were male while 45 (45%) were female of which major age group was 65-70 years of age (64%) while only 1% belong to the age group of 86-90. Minimum age was 65 years and maximum age was 86 years.
During clinical presentation different symptoms encountered, among which breathlessness (45%) was the most common followed by giddiness (39%), altered sensorium (29%), vomiting (27%), fever (18%), convulsion (17%), pedal oedema (17%) and others were headache, chest pain, decreased urine output, palpitation and easy fatiguability.
The most common condition observed among geriatric patients is cerebrovascular stroke (31%) followed by acute left ventricular failure (LVF) (19%), acute exacerbation of chronic obstructive pulmonary disease (COPD) (14%) and idiopathic pulmonary hemosiderosis (IPH) (11%) and others acute kidney injury, hypoglycaemia, hypertensive urgency, community acquired pneumonia, etc (Table 1).
Table 1: Analysis of final diagnosis among geriatric patients.
|
Diagnosis
|
No.
|
%
|
|
CV stroke
|
31
|
31
|
|
Acute LVF
|
19
|
19
|
|
Acute exacerbation of COPD
|
14
|
14
|
|
Intraparenchymal hemorrhage
|
11
|
11
|
|
Acute kidney injury on chronic kidney disease
|
9
|
9
|
|
Hypoglycemia
|
8
|
8
|
|
Hypertensive urgency
|
3
|
3
|
|
Community acquired pneumonia
|
2
|
2
|
|
Atrial fibrillation with fast ventricular rhythm
|
1
|
1
|
|
Hematemesis
|
1
|
1
|
|
Hepatic encephalopathy
|
1
|
1
|
Hypertension was the most common co-morbidity seen in patients (44) followed by hypertension and diabetes (40), COPD (15), ischemic heart disease (IHD) (15), diabetes (6), hypothyroidism (2) out of which 4,2,1 and 1 were noncompliant to medicine respectively (Figure 1).
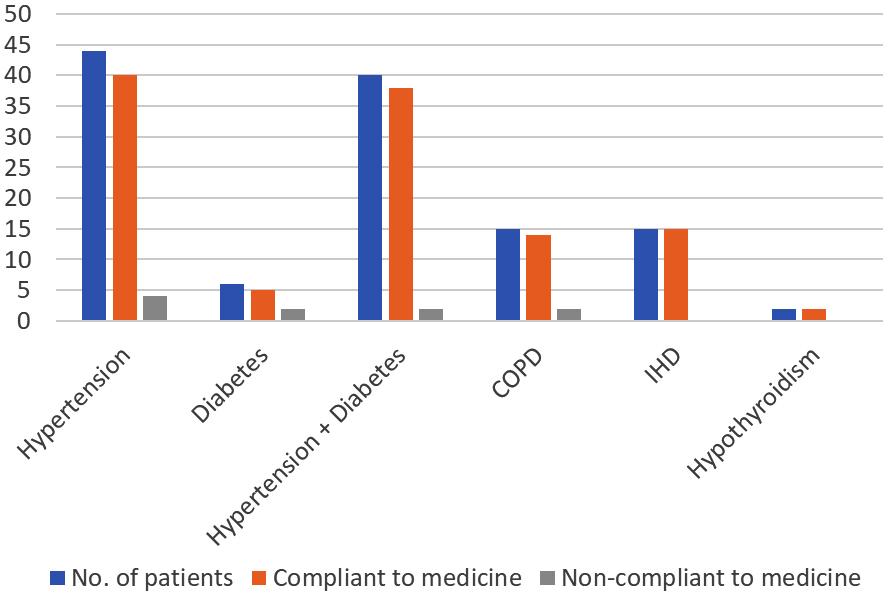
Figure 1: Co-morbidities among geriatric patients in relation with compliance to medicine.
Hypertension was associated with cerebral vascular (CV) stroke in 28 patients, acute LVF in 17 patients and IHD in 11 patients, while diabetes mellitus was associated with acute LVF in 12 patients, CV stroke in 11 patients and IHD in 7 patients. In patients having both hypertension and diabetes mellitus - CV stroke, acute LVF and IHD was seen among 11,11 and 5 patients respectively. Hypertension was the most common disease associated with CV stroke, acute LVF and IHD (Figure 2).
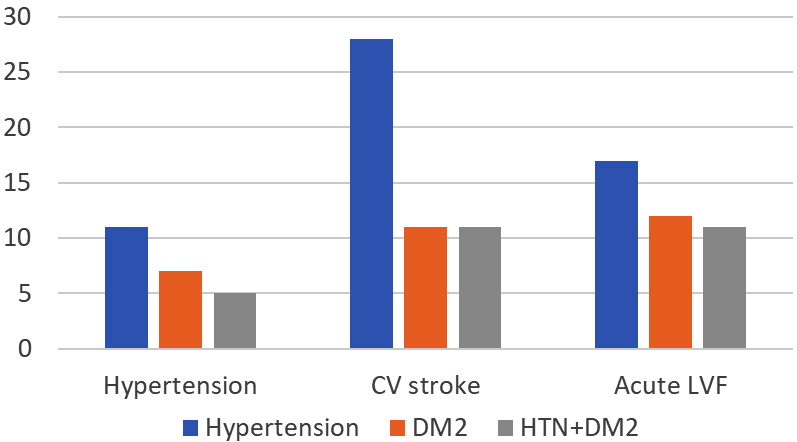
Figure 2: Relation of hypertension and diabetes with different clinical presentation.
Hypertension was found among 85.5% of male and 82.2% of female geriatric patients. However, this difference is not statistically significant. Diabetes was found among 41.8% of male and 51.1% of female geriatric patients. IHD was found among 16.4% of male and 13.3% of female geriatric patients. COPD was found among 20% of male and 8.9% of female geriatric patients. Hypothyroidism was found among 1.8% of male and 2.2% of female geriatric patients (Table 2).
Table 2: Male female wise distribution of co-morbidities among geriatric patients (N=100).
|
Comorbidity
|
Male (N=55)
|
Female (N=45)
|
p value
|
|
HTN
|
47(85.5)
|
37(82.5)
|
0.66
|
|
Diabetes
|
23(41.8)
|
23(51.1)
|
0.35
|
|
IHD
|
9(16.4)
|
6(13.3)
|
0.67
|
|
COPD
|
11(20)
|
4(8.9)
|
0.69
|
|
Hypothyroidism
|
1(1.8)
|
1(2.2)
|
0.88
|
There is no statistically significant difference in mean values of RBS, Hb, s. sodium, s. potassium, s. protein and s. albumin between male and female geriatric patients. T test is applied to compare mean values of above investigations between male and female as these values follow normal distribution as evident by Kolmogorov Smirnov and Shapirowilk tests which were applied priorly (Table 3).
Table 3: Investigations among geriatric patients (N=100).
|
Investigations
|
Male
|
Female
|
Independent T test
|
|
Mean
|
SD
|
Mean
|
SD
|
|
RBS mg/dl
(N=99)
|
187.84
|
55.35
|
184.48
|
71.35
|
t value=0.26
p value=0.79
|
|
Hb g/dl
(N=94)
|
11.22
|
2.19
|
11.71
|
2.46
|
t value=1
p value=0.31
|
|
S. sodium mMol/L (N=93)
|
134.63
|
6.3
|
134.4
|
6.37
|
t value=0.71
p value=0.86
|
|
S. potassium mMol/L (N=93)
|
4.13
|
0.92
|
4.33
|
0.7
|
t value=-1.14
p value=0.25
|
|
S. protein (N=77)
|
5.77
|
1.18
|
6.13
|
0.94
|
t value=-1.44
p value=0.15
|
|
S. albumin (N=77)
|
2.87
|
0.77
|
3.09
|
0.66
|
t value=-1.27
p value=0.20
|
Serum glucose levels increase proportionally to age, while glucose tolerance is decreasing. The reference range of fasting glucose is wider in the elderly (3.9 – 6.7 mmol/l). However, blood glucose levels were often low due to decreased body weight and dietary problems. Simultaneously serum insulin levels also increase indicating insulin resistance; this is responsible for impaired glucose tolerance observed in up to 25% of patients above 75 years.
Simultaneously with aging the level of some specific proteins, particularly that of albumin decrease (leading to a decrease of total protein levels). This is partly due to impairment of liver functions and an inappropriate diet. As albumin is the major carrier protein in blood, you should not be surprised, if a patient with low albumin levels presents with low calcium or hormone levels.
There is statistically significant difference in median values of s. creatinine, total bilirubin, direct bilirubin and ALT between male and female geriatric patients (p<0.01). All these values are higher in male as compared to female. Mann Whitney U test is applied to compare median values of above investigations between male and female as these values doesn’t follow normal distribution as evident by Kolmogorov Smirnov and Shapirowilk tests which were applied priorly (Table 4).
Table 4: Investigations among geriatric patients (N=100).
|
Investigations
|
Male
|
|
Female
|
|
Mann Whitney U test
|
|
Median
|
IQR
|
Median
|
IQR
|
|
Total count
(N=94)
|
11800
|
8550
|
10900
|
7198
|
Z value=-0.82
p value=0.41
|
|
Platelet count
(N=94)
|
40100
|
109600
|
27600
|
50250
|
Z value=-0.66
p value=0.5
|
|
ESR (N=85)
|
51
|
59
|
50
|
52
|
Z value=-0.08
p value=0.93
|
|
S. creatinine (N=93)
|
1.53
|
2
|
1.46
|
1
|
Z value=-2.76
p value<0.01
|
|
Total bilirubin (N=92)
|
0.86
|
1
|
0.65
|
1
|
Z value=-2.42
p value<0.05
|
|
Direct bilirubin (N=92)
|
0.4
|
0
|
0.37
|
0
|
Z value=-2.66
p value<0.01
|
|
ALT (N=93)
|
24
|
17
|
17.3
|
8
|
Z value=-2.74
p value<0.01
|
|
AST (N=83)
|
32
|
30
|
28
|
24
|
Z value=-1.74
p value=0.08
|
The ESR is increasing proportionally with age (in general by 0.22 mm/h per year above 20 years of age), but its exact cause is not known. Therefore, the upper limit of reference range in the elderly is 40 mm/h and 45 mm/h in males and females, respectively.
87% of diabetics had also hypertension as compared to 81.5% non-diabetics who were suffering from hypertension. However, there is no statistically significant relation between diabetes and hypertension.
Discussion
Among study participants, 55% of geriatric patients were males and 45% were females. M:F ratio was 1:0.81. In similar studies done by Reddy et al [4] and Ramadevi et al [5], found that 132 (66%) males and 68 (34%) females and 156 (67%) males and 78 (33%) females respectively.
Age group wise distribution shows that 64% of geriatric patients in present study were from 65 to 70 years group followed by 22% in 71 to 75 years 9% from 76 to 80 years, 4% from 81-85 years and 1% from 86-90 years group. Age group wise distribution shows that 64% of geriatric patients in present study were from 65-70 years group followed by 22% in 71 to 75 years 9% from 76 to 80 years,4% from 81-85 years and 1% from 86-90 years group. Mean age of patients was 70.36 years and SD is 5.18. Minimum age was 65 years and maximum age was 86 years. In a similar study conducted by Reddy et al [4], it was demonstrated that most of the patients were in the age group 65-69 years (n=62,31%); followed by 70-74years (n=58, 29%); 75-79 years (n=34)17%); 80-84 years (n=18, 9%), 60-64 years (n=14, 7%); 85- 89 years (n=10, 5%); and 90- 95 years (n=4, 2%) [5]. Sudarshan et al in their similar study conducted in Puducherry reported that Majority (59.2%) of the elderly were in the age group of 60-69 followed by 33.6% in 70-79 and 7.2% in 80 and above [6]. Subramanyam et al in their study, which was community base health care for the elderly in Pondicherry showed 66%, 25% and 8% for the ages 60 -69, 70 – 79 and 80 – 89 respectively [7]. So, the demographic data were comparable with the other studies.
During clinical presentation different symptoms encountered, among which breathlessness (45%) was the most common followed by giddiness (39%), altered sensorium (29%), vomiting (27%), fever (18%), convulsion (17%), pedal oedema (17%).
The most common condition observed among geriatric patients is cerebrovascular stroke (31%) followed by acute LVF (19%), acute exacerbation of COPD (14%) and IPH (11%). According to study done by Ramadevi et al., most common disease observed is cerebrovascular accidents with risk factor of un-controlled HTN (n=81, 34.6%), followed by chronic kidney disease (32,13.6%), coronary artery diseases with congestive cardiac failure observed in 19 patients (8.1%) [5]. Hyponatremia was not seen in any geriatric patients having vomiting and altered Sensorium as a presenting complains.
Hypertension was associated with CV stroke in 28 patients, acute LVF in 17 patients and IHD in 11 patients, while diabetes mellitus was associated with acute LVF in 12 patients, CV stroke in 11 patients and IHD in 7 patients. In patients having both hypertension and diabetes mellitus - CV stroke, acute LVF and IHD was seen among 11, 11 and 5 patients respectively. Hypertension was the most common disease associated with CV stroke, acute LVF and IHD.
45 patients presented with breathlessness, highest number of patients (19) had acute LVF. 39 patients presented with giddiness, highest number of patients (15) had ischemic stroke. 29 patients presented with altered sensorium, highest number of patients (11) had IPH. 27 patients presented with Vomiting, highest number of patients (12) had ischemic stroke. Hypertension (44) and hypertension and diabetes (40) together were the commonly encountered co-morbidities. Most patients with co-morbidities were found complaint to their medicines.
There is no statistically significant difference in mean values of RBS, Hb, s. sodium, s. potassium, s. protein and s. albumin between male and female geriatric patients. There is statistically significant difference in median values of s. creatinine, total bilirubin, direct bilirubin and ALT between male and female geriatric patients (p<0.01). All these values were higher in male as compared to female.
Among study participants, 87% of diabetics had also hypertension as compared to 81.5% nondiabetics who were suffering from hypertension. Most common condition observed among geriatric patients is cerebrovascular stroke (31%) followed by acute LVF (19%).
Kapil et al in their study demonstrated that a total of 8.6% (86/994) geriatric subjects had both HTN and DM. This concomitant prevalence of HTN and DM was higher in female (58.1%) compared with male (41.9%) [8]. Further in their study Kapil et al demonstrated that Age, education, income, tobacco consumption, MNA, physical activity, and BMI were found to be significantly associated with HTN (p < 0.05). The prevalence of HTN was found to be higher (58.5%) in subjects who were doing irregular physical activity than those who were doing regular physical activity (41.5%) [8].
Most common condition observed among geriatric patients were cerebrovascular strokes followed by acute LVF, these may be most common acute medical illness in geriatric population is due to the chronic co-morbid conditions. So according to this study, most common acute medical illness in geriatric population is due to the chronic co-morbid conditions. It is crucial to maintain chronic morbidity in a timely manner to minimize the complication. In our study, most common co-morbid conditions are hypertension diabetes and ischemic heart disease.
Elderly patients often experience functional decline following acute medical care due to delayed recovery. This functional decline may lead to permanent disability, which will increase the burden on the medical and long-term care systems, families, and society as a whole. Post-acute care may be aimed to promote the functional recovery of older adults, prevent unnecessary hospital readmission, and avoid premature admission to a long-term care facility.
Keeping elderly people in mind, geriatric OPD is also being run in our Civil Hospital, Ahmedabad. Beds are also reserved for geriatric patients in each ward in every department in our Civil Hospital, Ahmedabad. Care for the frail elderly is not simply a priority but it is our duty in 21st century.
Limitations of the study: The study population should be more for final conclusion and application to the general population.
Conclusion
The physicians play a key role in identifying the atypical presentation of acute illness in elderly patients with comorbidity and the prevention and management of related complications. Improvement in standard of living and health care facility has increased mean age of living of an individual. Under National Programme for Health Care of the Elderly (NPHCE) has envisaged to provide promotional, preventive, curative and rehabilitative services in an integrated manner for the elderly in various government health facilities, the range of services will include health promotion, preventive services, diagnosis and management of geriatric medical problems, day care services, rehabilitative services and home based care as needed.
Conflicts of interest
Authors declare no conflicts of interest.