Orginal Research
2024
March
Volume : 12
Issue : 1
Evaluation of clinical and radiological correlation in blunt trauma abdomen
Verma S, Aggarwal S, Verma A, Garg P, Yadav SK, Kumar D, Jangra A
Pdf Page Numbers :- 45-48
Surender Verma1,*, Shivika Aggarwal1, Anjali Verma2, Pradeep Garg1, Sunil Kumar Yadav1, Dinesh Kumar1 and Amit Jangra1
1Department of General Surgery, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Rohtak, Haryana 124001, India
2Department of Pediatrics, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Rohtak, Haryana 124001, India
*Corresponding author: Dr. Surender Verma, Associate Professor, Department of General Surgery, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Rohtak, Haryana 124001, India. Email: drsurn@gmail.com
Received 11 September 2023; Revised 7 November 2023; Accepted 21 November 2023; Published 30 November 2023
Citation: Verma S, Aggarwal S, Verma A, Garg P, Yadav SK, Kumar D, Jangra A. Evaluation of clinical and radiological correlation in blunt trauma abdomen. J Med Sci Res. 2024; 12(1):45-48. DOI: http://dx.doi.org/10.17727/JMSR.2024/12-8
Copyright: © 2024 Verma S et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Abdominal trauma is commonly encountered injury caused mainly due to road traffic accidents (RTA). The research aimed to study the cases of abdominal trauma, its different modes of presentation and correlation of radiological and clinical findings with operative findings in these patients.
Material and methods: An observational study was conducted in a tertiary care institute. Hemodynamic instability and finding of shattered solid viscera on imaging and/or other injury requiring exploration were the criteria for surgical intervention. Radiological findings were then compared with the operative findings. In addition, clinical parameters were recorded till the patient was discharged and then analyzed.
Results: A total of 62 patients presenting in Trauma Centre with an antecedent history of blunt abdominal trauma. Most common age group affected was 21-40 years and mean age was 30.4 + 11.56 years. Males were more affected and RTA was the most common mode of injury. Associated injuries included chest injuries (20.9%), limb fracture (19.35%) and soft tissue injuries (4.83%). Twenty patients were operated and rest of patients were managed conservatively. Sensitivity of USG in detecting liver and splenic injuries was 100% and specificity was 92.3% and 92.8% respectively. Sensitivity of CT for detecting injury to liver, spleen, renal, pancreas and small bowel was 100%, 83.3%, 100%, 100% and 83.3% and specificity was 100% in all injuries. Mortality rate in our study was 4.83%.
Conclusion: High degree of suspicion and prompt screening by radiological investigations of patients should be done to rule out intraabdominal injury. Necessary investigations and early surgery whenever required is the key to management of blunt trauma patients.
Keywords: blunt trauma; radiology; solid viscera injury
Full Text
Introduction
Abdominal trauma is one of the commonly encountered injuries in surgical emergency and maximum of them are blunt in nature [1]. Blunt trauma abdomen is mainly due to motor vehicle accidents and can also because of assault, fall, sport injuries or any other kind of mishaps [2].
Blunt abdominal trauma (BTA) is usually not obvious and can be often missed. Delay in diagnosis and inadequate treatment of the abdominal injuries can be fatal. Our understanding in the management of blunt abdominal trauma is progressively increasing. In spite of the best techniques and advances in diagnostic and supportive care, the morbidity and mortality still remain large. Study of literature reveals that in today’s era, such deaths can become negligible if early identification of the problem is done and line of management is decided. In recent past many changes in the treatment of patients with blunt abdominal trauma, have been taking place. Traditionally, emergency laparotomy was the procedure of choice, currently conservative management is the most common management strategy in hemodynamically stable patients [3, 4]. Many surgeons are still suspicious of this approach because of the possibility of missed abdominal injuries, delayed recognition of significant intra-abdominal bleeding and associated mismanagement of the patient. It is appropriate for physicians and surgeons to have a healthy skepticism of new techniques until the value of a new approach have been documented and the appropriate patients for such therapies are clearly defined.
Most commonly injured solid organs in BTA are liver and spleen followed by kidney, pancreas, bowel and mesentery and vascular injuries [5]. Abdominal computed tomography (CT) has become the mainstay of imaging for the stable BTA patient and has led to the emergence of non-operative management of many solid abdominal organ injuries. The use of CT has helped to decrease the total number of laparotomies performed for abdominal trauma [6].
As prompt diagnosis of injury to both solid and hollow viscus is important for determining the outcome, we have done this study to see the pattern of BTA and to determine organ wise specificity and sensitivity of radiological investigations (USG and CT scan) by correlating them with the intraoperative findings.
Material and methods
A Prospective observational study was conducted in the Department of General Surgery at a Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Rohtak from August 2019 to July 2021 after clearance of the ethical committee approval. Patients presenting in the emergency department with blunt trauma abdomen having significant findings on USG and CT abdomen were recruited in this study. Pregnant females and those not giving consent for study were excluded.
All patients clinically suspected of having blunt trauma abdomen were thoroughly examined and a detailed history was taken after adequate resuscitation of the patient in accident and emergency department based on advanced trauma life support. General physical examination was done, associated injuries and signs suggestive of blunt trauma abdomen such as tenderness, guarding, contusions or abrasions over the abdomen were noted. Patients who were hemodynamically stable were considered for ultrasonography and CT abdomen. The decision for operative or non-operative management was based on the clinical examination and results of diagnostic tests. Hemodynamic instability and finding of shattered solid viscera on imaging and/or other injury requiring exploration were the criteria for surgical intervention. Patients kept on conservative management and all findings were recorded till the patient was discharged. All findings were recorded, tabulated & analyzed.
Results
A total of 62 patients of BTA were enrolled over a period of 2 years. Most common age group affected was 21-40 years in which males were more affected. RTA was the most common mode of injury (Table 1). Most common organ injured was liver in 50% of patients followed by spleen in 33.3% of patients as per CT findings. Associated injuries included chest injuries (20.96%), limb fractures (19.35%) and soft tissue injuries (4.83%). Ultrasonography showed free fluid in 60 patients (96.77%). However, the organ injured was described only in 20 patients (32.25%). CT scan showed pneumoperitoneum in 3 patients (4.83%), hemoperitoneum in 50 patients (80.64%) and both in 4 patients (6.45%).
Mostly patients (42) were managed conservatively (Table 1) and 20 patients were operated. USG was highly sensitive for detecting liver and splenic injuries. Specificity of USG in detecting injuries to liver, spleen and kidney was 100% however it was much less in injuries of pancreas (50%) and bowel (20%). Among the operated patients, CECT was able to detect liver injuries in 7 patients (Figure 1), splenic injuries in 5 patients (Figure 2), bowel injuries in 5 patients, pancreatic injury in 2 and renal injury in 1 patient. CT scan was high specificity for injuries of all the organs but relatively it is relatively less sensitive for splenic and bowel injuries (83.3%) (Table 2). Complications after surgery were there in 17.7% of patients. Mortality rate in our study was 4.83% (Table 1).
Table 1: Showing baseline demographic parameters of patients.
|
Parameters
|
Number of patients
|
|
Mean age (years)
|
30.4 + 11.56 years
|
|
Male: female ratio
|
9.3:1
|
|
Mode of injury [n (%)]
|
|
|
RSA
Assault
Fall from height
|
46 (74.2%)
5(8.1%)
11(17.7%)
|
|
|
Mean Length of stay in hospital (days)
|
10.6 days+ 8.1 days
|
|
Presenting features [n (%)]
|
|
|
Pain
Obstipation
Distension
Vomiting
Haematuria/Anuria
|
60 (96.8%)
10 (16.1%)
16 (25.8%)
9 (14.5%)
1 (3.22%)
|
|
Management [n (%)]
|
|
|
Operative
Conservative
|
20 (32.3%)
42 (67.7%)
|
|
Complications [n (%)]
|
|
|
Wound complications
Bedsores
Cardiopulmonary complications
|
6 (9.7%)
1 (1.6%)
4 (6.4%)
|
|
Outcome [n (%)]
|
|
|
Discharged
Expired
|
59 (95.2%)
3 (4.8%)
|
Table 2: Showing correlation between clinical, radiological and intraoperative findings in 20 operated patients.
|
Organ injured
|
Clinical findings (n)
|
Intraoperative finding (n)
|
CT
(n)
|
Sensitivity
|
Specificity
|
USG
(n)
|
Sensitivity
|
Specificity
|
|
Liver
|
7
|
7
|
7
|
100%
|
100%
|
8
|
100%
|
92.3%
|
|
Spleen
|
6
|
6
|
5
|
83.3%
|
100%
|
7
|
100%
|
92.8%
|
|
Renal
|
1
|
1
|
1
|
100%
|
100%
|
1
|
100%
|
100%
|
|
Pancreas
|
0
|
2
|
2
|
100%
|
100%
|
1
|
50%
|
100%
|
|
Bowel and mesentery
|
2
|
6
|
5
|
83.3%
|
100%
|
1
|
20%
|
100%
|
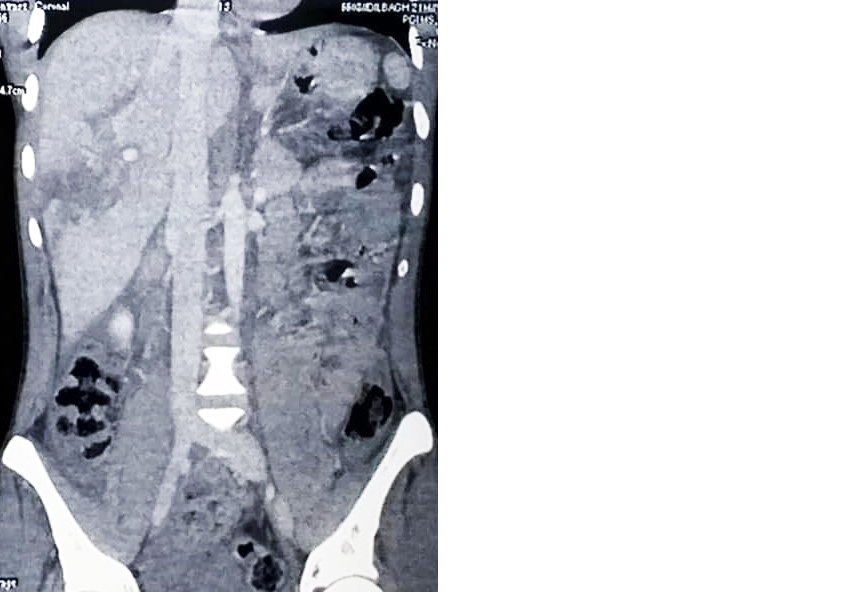
Figure 1: Coronal view of CECT abdomen showing Grade 3 liver injury.
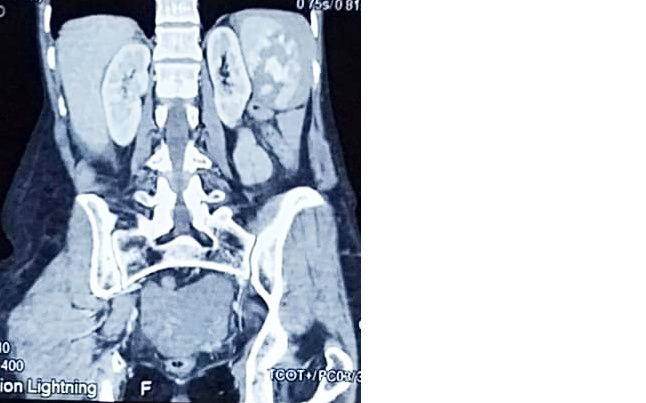
Figure 2: Coronal view of CECT abdomen showing Grade 4 splenic injury.
Discussion
Evaluating patients who have sustained blunt abdominal trauma remains one of the most challenging and intensive aspects of acute trauma care. It is necessary that the early recognition and effective management of these injuries are essential for the survival and prevention of far-reaching complications [7].
In our study, majority of patients are in the young age group. Most of the patients in all the previous studies were of younger age group probably due to reason that young people are more involved in the outdoor activity and have high tech lifestyle [8-10]. Males outnumbered females which is comparable to other peer studies probably because males are mainly involved in outdoor activities, assault and violent crimes [8]. Due to rapid and unprecedented motorisation combined with the safety environment, active outdoor life, fast driving vehicles, aggressive behaviour and probably under influence of alcohol, RTA is more common day by day so it is the more common mode of injury in our study.
The presenting complaints of the patients were pain abdomen, non-passage of stool and flatus, vomiting, abdominal distension and/or hematuria or anuria. However, in almost all the patients’ pain was the main feature which is in concordance with other studies [11, 12].
Most common associated injuries encountered were chest injuries followed by orthopaedic and soft tissue injuries. Study done by Mehta et al was also having similar findings. This could be because intraabdominal organs especially liver and spleen are subdiaphragmatic in location, relatively immobile and encaged within lower ribs. In present study, commonly involved organ is liver followed by spleen, bowel, pancreas and kidney. The current study is at par with other peer studies in which liver is the most commonly affected organ because of its sub diaphragmatic location and relative immobility [8, 9, 13].
USG detected free fluid in maximum number of patients. USG was highly sensitive in detecting liver, spleen and renal injury but was less sensitive for pancreatic as well as bowel injuries. This investigation has over detected liver and splenic injury in 2 patients.
It has been seen in previous literature that abdominal CT is highly sensitive and specific for early diagnosis of splenic as well as hepatic injury [14, 15]. In our study, CT has reliably detected liver, pancreas and renal injuries but it was relatively less sensitive for splenic and bowel injuries. Similar results were seen in a study conducted by Wing et al which showed sensitivity of CT in detecting liver injuries is 100% and splenic injuries is 86.6% [16]. CT is a proven diagnostic modality in detecting bowel injuries with a sensitivity of 70-95% and specificity of 92-100% [17]. One patient had mesenteric tear which could not be picked on CT scan and another one had small subcapsular hematoma of spleen which was an incidental finding in one of our patients of traumatic bowel injury. Hence stable patients who are kept on conservative management should be monitored clinically along with serial CT scan to detect missed mesenteric injury which can lead to gangrene of the bowel. In addition, studies which highlight impact of variables like clinical judgement on CT scan rates in various centres can provide more insight into the decision-making policies [18].
Treatment strategy mainly depends on grade of injury, hemodynamic stability of patient, clinical and radiological findings. In an Indian study done by Amuthan et al [19], 42% of the patients were managed conservatively while 58% were managed by operative procedures. However, in our study maximum patients were managed conservatively because of good patient monitoring, availability of experienced surgeon and radiologist and well-equipped infrastructure. The postoperative complications as well as mortality rate were consistent with previous studies [9, 11].
Conclusion
High degree of suspicion and prompt screening of patients should be done to rule out any intraabdominal injury. USG abdomen is a very sensitive method for screening of patients with suspected abdominal injury. CT is a sensitive and specific method for detecting the organ injured and extent of injury and it also helps in making a decision for operative or conservative management. Larger studies are required to establish correlation of CT findings with specific organ injuries particularly mesenteric injuries.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016; 65:1–96.
[2] Isenhour JL, Marx J. Advances in abdominal trauma. Emerg Med Clin North Am. 2007; 25:713–33.
[3] Raza M, Abbas Y, Devi V, Prasad KV, Rizk KN, et al. Non operative management of abdominal trauma–a 10 years review. World J Emerg Surg. 2013; 8:1–6.
[4] Schroeppel TJ, Croce MA. Diagnosis and management of blunt abdominal solid organ injury. Curr Opin Crit Care. 2007; 13:399–404.
[5] Larsen JW, Søreide K, Søreide JA, Tjosevik K, Kvaløy JT, et al. Epidemiology of abdominal trauma: An age- and sex-adjusted incidence analysis with mortality patterns. Injury. 2022; 53:3130–3138.
[6] Hamidi MI, Aldaoud KM, Qtaish I. The role of computed tomography in blunt abdominal trauma. Sultan Qaboos Univ Med J. 2007; 7:41–46.
[7] Jolley S, Upadhyay M, Jain RL. Blunt abdominal trauma. A clinical study of 100 cases. Ind J Sur. 1993; pp.209–203.
[8] Panchal HA, Ramanuj AM. The study of abdominal trauma: Patterns of injury, clinical presentation, organ involvement and associated injury. Int Surg J. 2016; 3:1392–1398.
[9] Mehta N, Babu S, Venugopal K. An experience with blunt abdominal trauma: evaluation, management and outcome. Clin Pract. 2014; 4:34–37.
[10] Ortiz CA, Hughes V, Ramallo D. Gastric perforation after blunt abdominal trauma: first case report in Argentina. J Surg Case Rep. 2022; 2022:rjac394.
[11] Solanki HJ, Patel HR. Blunt abdomen trauma: a study of 50 cases. Int Surg J. 2018; 5:1763–1769.
[12] Tripathi MD, Srivastava RD, Nagar AM, Pratap VK, Dwivedi SC. Blunt abdominal trauma with special reference to early detection of visceral injuries. Indian I Surg. 1991; 53:179–184.
[13] Aziz A, Bota R, Ahmed M. Frequency and pattern of intra-abdominal injuries in patients with blunt abdominal trauma. J Trauma Treat. 2014; 3:196.
[14] Larsen JW, Thorsen K, Søreide K. Splenic injury from blunt trauma. Br j Surg. 2023; 110:1035–1038.
[15] Dixe I, Sailer A, Solomon N, Borse R, Cavallo JJ, et al. Grading Abdominal Trauma: Changes in and Implications of the Revised 2018 AAST-OIS for the Spleen, Liver, and Kidney. Radiographics. 2023; 43:e230040.
[16] Wing VW, Federle MP, Morris Jr JA, Jeffrey RB, Bluth R. The clinical impact of CT for blunt abdominal trauma. Am J Roentgenol. 1985; 145:1191–1194.
[17] Panda A, Kumar A, Gamanagatti S, Das R, Paliwal S, et al. Can multidetector CT detect the site of gastrointestinal tract injury in trauma?–A retrospective study. Diagn Interv Radiol. 2017; 23:29.
[18] Hassankhani A, Valizadeh P, Amoukhteh M, Jannatdoust P, Saeedi N, et al. Disparities in computed tomography utilization for pediatric blunt trauma: a systematic review and meta-analysis comparing pediatric and non-pediatric trauma centers. Emerg Radiol. 2023; 30:743–764.
[19] Amuthan J, Vijay A, Pradeep C, Anandan H. A clinical study of blunt injury abdomen in a tertiary care hospital. Int J Sci Study. 2017; 5:108–112.