Abstract
Background: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its variants have instigated the global COVID-19 pandemic, which unfolded in waves over nearly three years since its emergence in 2019. Variances in host immune responses have resulted in a spectrum of symptoms ranging from asymptomatic to mild, moderate, severe pneumonia-like, or critical conditions. For many individuals, symptomatic conditions exacerbated and posed life-threatening risks, particularly when co-morbidities such as diabetes mellitus, chronic obstructive pulmonary disease (COPD), cardiovascular diseases (CVD), hypertension, malignancies, and HIV were present. This study was aimed to ascertain the co-morbidity trends across the two major waves of COVID-19.
Method: In India, COVID-19 patients from the first wave (April 1, 2020 to January 31, 2021) and the second wave (March 1, 2021 to October 1, 2021) were categorized into asymptomatic, moderate, severe, and critical groups, with 100 patients in each category. These patient groups were further subdivided based on co-morbidities and subjected to data analysis.
Results: Diabetes mellitus, hypertension, and lung complications were identified as common co-morbidities significantly impacting the quality of life for COVID-19 patients.
Conclusions: Our data analysis has highlighted the influence of co-morbidities or multi-morbidities in exacerbating severe and critical conditions during both waves 1 and 2 of COVID-19 infections.
Keywords: co-morbidities; COVID-19; diabetes mellitus; hypertension; lung complications
Full Text
Introduction
The global impact of COVID-19 and its unchecked transmission has caused profound devastation, escalating economic burdens, and increased mortality worldwide. According to the WHO report and data analysis, more than 69 million deaths have been attributed to COVID-19 infections and its variants, occurring in successive waves. The global population has faced distinct waves of COVID-19 infections, each characterized by unique attributes. The initial wave, spanning from April 1, 2020 to January 31, 2021, witnessed a gradual and steady spread that resulted in significant fatalities. In contrast, the second wave, occurring between March 1, 2021, and October 1, 2021, featured rapid and widespread transmission, accompanied by alarming mortality rates [1, 2].
COVID-19 has profoundly impacted a vast population across multiple waves, influenced by various factors including the emergence of distinct mutant variants with varying virulence, host immune responses, and co-morbidities [3]. Subsequent to the initial wave, the virus underwent mutations, leading to the emergence of several variants such as Alpha, Beta, Delta, and Omicron. In India, Beta and Delta variants were predominant during the second wave [4]. Consequently, the second wave resulted in more severe consequences in terms of mortality and a global economic slowdown. Similar to global trends, India witnessed a higher mortality rate during the second wave compared to the first, with a total of 530,000 deaths attributed to COVID-19 infections [5].
Co-morbid conditions are significant predictors of COVID-19 severity and critical illness, with their impact on COVID-19-related mortality being notable in both the first wave and more pronounced in the second wave [6]. Studies indicate that increased angiotensin converting enzyme II (ACE2) expression, combined with co-morbidities, enhances viral entry. Certain co-morbidities show heightened ACE2 receptor expression and increased protein convertase activity, facilitating viral entry into host cells [7]. Common co-morbidities among COVID-19 patients include hypertension, diabetes mellitus, and lung complications [6].
Due to COVID-19's affinity for the nervous system, individuals with neurological disorders are especially vulnerable to respiratory infections [8]. Patients with diabetes mellitus are at higher risk of experiencing severe illness, requiring intensive care unit (ICU) admission, and facing increased mortality due to COVID-19. Similarly, those with chronic obstructive pulmonary disease (COPD) face elevated risks of severe complications and critical outcomes following COVID-19 infections [6].
This study aims to explore how co-morbidities influence the severity of COVID-19 patients during India's first and second waves.
Methods
Study population and data collection
During the first wave (April 1, 2020, to January 31, 2021) and the second wave (March 1, 2021, to October 1, 2021) of the COVID-19 pandemic, individuals presenting symptoms suggestive of COVID-19 sought medical attention at KIMS Hospitals for diagnostic purposes and were enrolled in the study. Nasopharyngeal and/or oropharyngeal swabs were collected from these patients and preserved in lysis buffer solution following World Health Organization (WHO) guidelines. The lysed samples underwent further processing using real-time quantitative polymerase chain reaction (RT-qPCR) to confirm the presence of SARS-CoV-2. Positive and negative cases across all age groups were retrospectively collected and classified into five study groups based on symptoms, in accordance with guidelines from the WHO and the Indian Council of Medical Research (ICMR). These groups included negative (control), asymptomatic, moderate, severe, and critical, each comprising 100 cases, and totaling 500 patients from each wave. This study was approved by the Institutional Ethics Committee at KIMS Hospital, Secunderabad, India (KIMS/ECBMHR/2021/23-01), and was conducted in accordance with the principles outlined in the Declaration of Helsinki 2.0.
Data analysis
Data analyses were performed using Microsoft Excel. Results are presented as percentages and represented either as medians with ranges or as means ± standard error of the mean (SEM) or ± standard deviation (SD).
Results
Characteristics of COVID-19 patients
COVID-19 patients who visited KIMS Hospitals during wave 1 (April 1, 2020, to January 31, 2021) and wave 2 (March 1, 2021, to October 1, 2021) were examined. Significant increases in pulse rate, respiratory rate, white blood cell count, procalcitonin, and creatinine levels were observed in severe and critical patients compared to negative and asymptomatic groups (Figure 1a-d, & e). Moderate patients also showed notable increases in these parameters compared to negative and asymptomatic groups.
However, parameters such as partial pressure of oxygen, hemoglobin levels, platelet count, and glomerular filtration rate (GFR) were significantly lower in moderate, severe, and critical patients compared to negative and asymptomatic groups (Figure 1f-h & i).
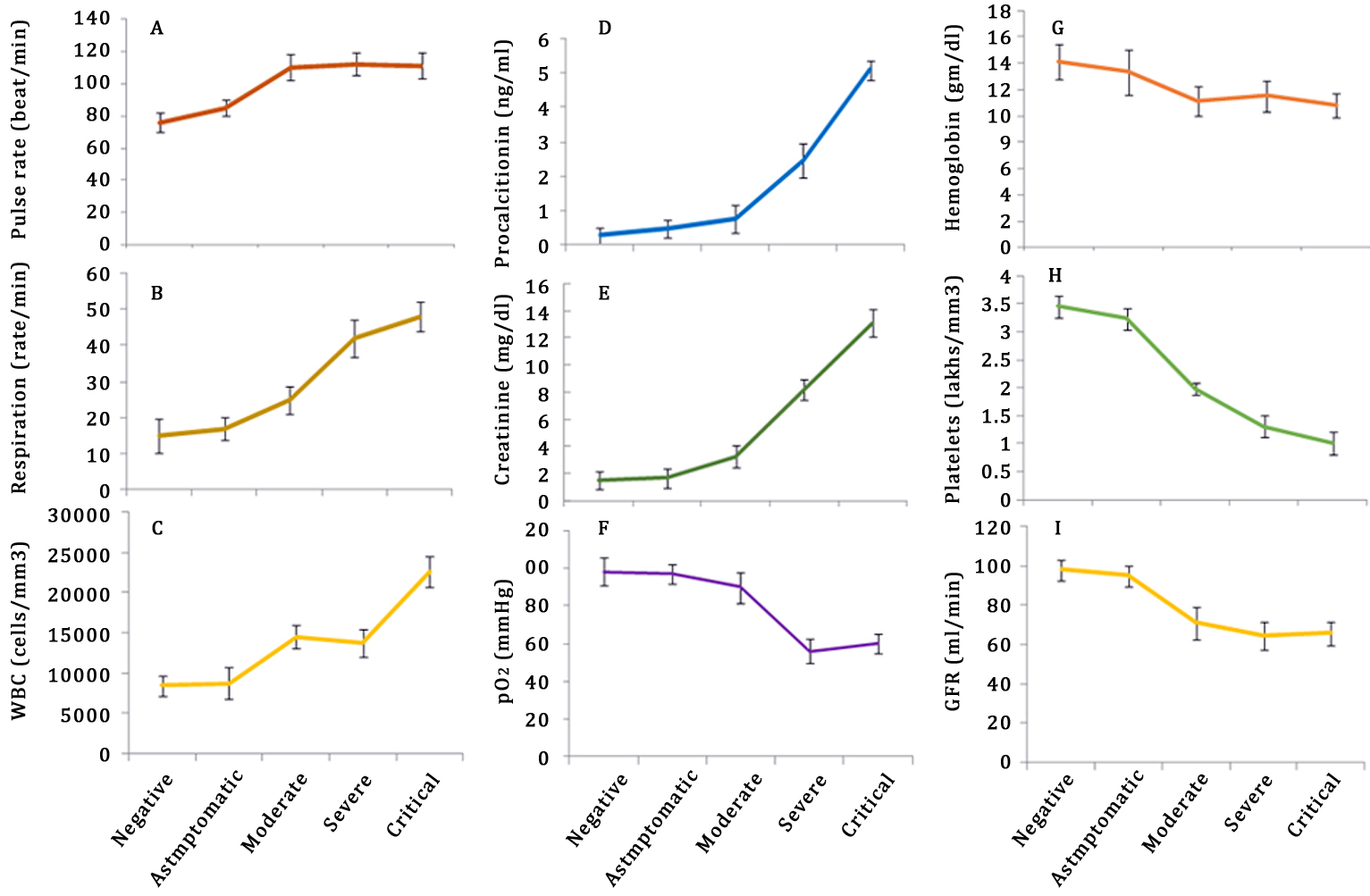
Figure 1: Characteristics of COVID-19 patients. COVID-19 patients visiting KIMS hospitals during waves 1 and 2 underwent examination, with their clinical parameters including pulse rate (a), respiration rate (b), white blood cell count (c), procalcitonin levels (d), creatinine levels (e), partial pressure of oxygen (f), hemoglobin levels (g), platelet count (h), and glomerular filtration rate (i) recorded across negative, asymptomatic, moderate, severe, and critical patient groups. Error bars indicating significance levels (p < 0.05) were included in each group.
Incidence of co-morbidities in wave 1 and wave 2
An incidence analysis conducted among asymptomatic, moderate, severe, and critical COVID-19 patients revealed that during wave 1, hypertension and diabetes were predominant co-morbidities among severe and critical patients (Figure 2a). Interestingly, during wave 2, in addition to hypertension and diabetes, other co-morbidities such as lung complications, obesity, renal disease, ischemic heart disease, and COPD were significantly more prevalent among severe and critical patients compared to negative and asymptomatic groups (Figure 2b).

Figure 2: Incidence of co-morbidities in wave 1 and wave 2. The prevalence of co-morbidities such as hypertension, diabetes, lung complications, COPD, obesity, etc., is depicted in bar diagrams for wave 1 (a) and wave 2 (b). Error bars indicating significance levels (p < 0.05) are included for each group.
Discussion
COVID-19 infections followed a periodic pattern, characterized by two main waves occurring from May 2019 to March 2021 and from March 2021 to April 2022 [9]. Data and statistics from the WHO indicate that the rate of infections and mortality was notably higher during the second wave compared to the first wave, both in India and globally. However, in subsequent waves of COVID-19 infections, there was a noticeable increase in secondary complications, including both new and existing co-morbidities [10]. The elevated mortality in the initial waves can be attributed to inadequate individual immune responses, insufficient anti-COVID-19 antibodies, and the presence of co-morbidities [11].
Our study examined the effects of COVID-19 infections on patients categorized by symptoms and the presence of pre-existing and new co-morbidities during waves 1 and 2. We found a direct association between the presence of co-morbidities and COVID-19 incidence in both waves, highlighting their potential impact on disease severity [10]. Diabetes mellitus and hypertension were identified as prominent co-morbidities that significantly contributed to the morbidity and mortality of patients throughout both waves.
Previous research has identified hypertension and diabetes as prevalent co-existing conditions in COVID-19 infections, alongside cardiovascular disease [12]. Our study supports these findings, revealing a higher occurrence of diabetes-related co-morbidities, particularly associated with severe and critical complications among COVID-19 patients, notably during wave 2. This trend may be attributed to the emergence of new diabetes cases and hypertension as secondary effects of COVID-19 infection during wave 1. Meta-analyses conducted by other researchers have also emphasized that co-morbidities significantly increase the risk of mortality and severity in COVID-19 patients [13].
Moreover, non-diabetic co-morbidities such as hypertension, lung disease, renal disease, and cardiovascular disease were observed more frequently in both waves, with a notably higher prevalence in wave 2, underscoring their significant role in exacerbating the severity and morbidity of patients [14]. Additionally, we identified other less common co-morbidities in both waves, including chronic obstructive pulmonary disease, chronic kidney disease, chronic liver disease, malignancy, and chronic neurological disease, which contributed to the worsening severity among COVID-19 patients, particularly during the second wave. This necessitated chaotic hospitalizations and called for aggressive management of COVID-19 patients.
Conclusion
This study examines how co-morbidities influence the outcomes of COVID-19 across different symptomatic categories, including asymptomatic, mild, moderate, severe, critically ill (survivors), and critically ill (deceased) groups. Both diabetic and non-diabetic co-morbidities have emerged as significant factors contributing to the severity and critical illness seen in COVID-19 patients. The higher mortality observed during wave 2 correlates strongly with an increased prevalence of co-morbidities compared to wave 1. Additionally, COVID-19 infections during wave 1 have contributed to the higher incidence of co-morbidities and mortality observed in wave 2. The emergence of various mutant variants of COVID-19 and the associated co-morbidities underscore the unpredictable nature of this virus. This highlights the need for robust surveillance systems to monitor and effectively manage such pandemics in the future.
Acknowledgement
We wish to extend our appreciation to Mrs. K. Ramamani for her invaluable help in collecting patient information. Funding Intramural funding from KIMS Foundation and Research Center (KFRC).
Conflict of interest
The authors declare no conflicts of interest.
References
[1] Tendulkar P, Pandey P, Panda PK, Bhadoria AS, Kulshreshtha P, et al. Comparative study between the first and second wave of COVID-19 deaths in India: A single center study. Cureus. 2023; 15:e37472.
[2] Goyal P, Sikary AK, Sachdeva RA, Parashar L, Tarique A. Mortality analysis of COVID-19 cases during the second wave and its comparison with the first wave: A hospital-based study. J Family Med Prim Care. 2022; 11:6091–6095.
[3] Farhud DD, Mojahed N. SARS-COV-2 notable mutations and variants: A review article. Iran J Public Health. 2022; 51:1494–1501.
[4] Mahapatra RK, Tiwari R, Sarangi AK, Sharma SK, Khandia R, et al. Twin combination of Omicron and Delta variants triggering a tsunami wave of ever high surges in COVID19 cases: a challenging global threat with a special focus on the Indiansubcontinent. J Med Virol. 2022; 94:1761–1765.
[5] Zirpe KG, Dixit S, Kulkarni AP, Pandit RA, Ranganathan P, et al. The Second- vs First-wave COVID-19: More of the Same or a Lot Worse? A Comparison of Mortality between the Two Waves in Patients Admitted to Intensive Care Units in Nine Hospitals in Western Maharashtra. Indian J Crit Care Med. 2021; 25:1343–1348.
[6] Jonaid AM, Sakeel A, Mrunal S, Mohammad HA, Saleh A, et al. The impact of COVID-19 on comorbidities: A review of recent updates for combating it. Saudi J Biol Sci. 2022; 29:3586–3599.
[7] Santra D, Banerjee A, De SK, Thatoi H, Maiti S. Relation of ACE2 with co-morbidity factors in SARS-CoV-2 pathogenicity. Comp Clin Path. 2023; 32:179–189.
[8] Veleri S. Neurotropism of SARS-CoV-2 and neurological diseases of the central nervous system in COVID-19 patients. Exp Brain Res. 2022 Jan; 240:9–25.
[9] Iftimie S, López-Azcona AF, Vallverdú I, Hernández-Flix S, de Febrer G, et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. PLoS ONE. 2021: 16:e0248029.
[10] Chatterjee S, Nalla LV, Sharma M, Sharma N, Singh A A , et al. Association of COVID-19 with Comorbidities: An Update. ACS Pharmacol Transl Sci. 2023; 6:334–354.
[11] DeWolf S, Laracy JC, Perales MA, Kamboj M, van den Brink MRM. SARS-CoV-2 in immunocompromised individuals. Immunity. 2022; 55:1779–1798.
[12] Jayaswal SK, Singh S, Malik PS, Venigalla SK, Gupta P, et al. Detrimental effect of diabetes and hypertension on the severity and mortality of COVID-19 infection: A multi-center case-control study from India. Diabetes Metab Syndr. 2021; 15:102248.
[13] Jindal R, Gupta M, Khan FR, Chaudhry G. Prevalence of co-morbidities and its association with mortality in Indian patients with COVID-19: A meta-analysis. Indian J Anaesth. 2022; 66:399–418.
[14] Shahidi S, Vahdat S, Atapour A, Reisizadeh S, Soltaninejad F. The clinical course and risk factors in COVID-19 patients with acute kidney injury. J Family Med Prim Care. 2022; 11:6183–6189.