Full Text
Introduction
Angiomyolipoma (AML) is a rare benign tumour originating from the perivascular cells of the smooth muscle and fat. It is typically found in the kidney but can also occur in extrarenal sites [1-3]. Cutaneous Angiomyolipoma is more rarely presented than the classical and the latter may be associated with Tuberous sclerosis syndrome, which is relatively less common in cutaneous angiomyolipoma. Surgical resection plays a major role in getting cured. Histopathological examination establishes the final diagnosis.
Case Report
This case report presents the case of a 59-year-old male patient from the Etawah district who presented with a lump in the anterior abdominal wall in the umbilical region for the past 5 months in the Out-patient Department of Radiation Oncology in Uttar Pradesh University of Medical Sciences, Saifai, Etawah. The patient was asymptomatic but was concerned about the nature of the lump and agreed to undergo excision of the lump, which revealed angiomyolipoma of the anterior abdominal wall on histopathological examination. The patient had no complications from excision and was discharged from the hospital. Till writing of this case report patient did not had any recurrence.
Discussion
Angiomyolipoma is a rare benign tumour that can also occur at extrarenal sites [4]. Classic AML is characterized as a benign mesenchymal neoplasm comprising mature adipose tissue, well-defined blood vessels with thick walls, and varying quantities of smooth muscle fibers. It is most common in the kidneys (99.7%) and is further classified as renal or extrarenal. There are several types of perivascular epithelioid cell tumors, and classic AML is one of them. Others in this family are lymphangioleiomyomatosis, clear cell "sugar" tumor, and clear cell myomelanocytic tumor of the falciform ligament or ligamentum teres. abdominopelvic sarcoma of PECs, and cutaneous PEComa.
Most classic AMLs are sporadic (80%), with up to 20% being associated with TSC, a rare, autosomal dominant, multisystemic syndrome characterised by cutaneous abnormalities. Biallelic mutations in TSC1 and TSC2 cause mTOR hyperactivation and stimulate cell growth. Sporadic AML has a female predilection (4:1) and occurs in patients between the ages of 40-60 years, while TSC-associated classic AML has no gender predominance and occurs in patients between the ages of 30-40 years.
Classic AML accounts for less than 1% of renal tumours but is the most common renal mesenchymal tumour. The majority of traditional renal angiomyolipomas (AMLs) are commonly asymptomatic and are usually discovered incidentally through imaging examinations, surgical procedures, or post-mortem examinations. Nevertheless, it is worth noting that more than 80% of those measuring more than 4 cm in diameter are associated with symptoms such as abdominal or flank pain, blood in the urine, nausea, vomiting, fever, palpable masses, renal failure, or new-onset hypertension.
Classic angiomyolipoma (AML) is a rare, benign tumor with varying proportions of thick-walled blood vessels, adipose tissue, and smooth muscle cell bundles similar to findings in our case study Figures 1,2,3. It is predominantly found in males (70%) with a wide age range (2-77 years). Clinically, benign vascular tumors (17%), lipomas (28%), and cystic lesions (35%), primarily epidermoid cysts, were the most common diagnoses.
Classic AML is typically positive for melanocytic markers (95%), such as HMB-45, Melan-A, Microphthalmia transcription factor, and tyrosinase. Additionally, smooth muscle cells exhibit immunoreactivity towards myogenic markers like desmin, calponin, and SMA. Treatment using mTORC1 inhibitors, like sirolimus, has been shown to prevent renal failure in certain cases and show positive clinical response. Patients with asymptomatic AMLs less than 1 cm and those with substantial comorbidities with AMLs less than 3 cm ought to undergo routine CT or MRI follow-up.
Cutaneous AML, previously termed cutaneous angiomyolipoma, is demographically, clinically, and immunohistochemically distinct from its classical counterpart. The majority of patients have no symptoms at all and only have a nodule that is palpable or visible and grows slowly. Some patients experience tumour size fluctuations over time or are associated with environmental temperature changes, pain, and obstructive symptoms related to specific sites and large tumour sizes.
Most of the time, cutaneous AMLs are mistakenly thought to be lipomas (28% of the time), cystic lesions (35% of the time, mostly epidermoid cysts), or benign vascular tumors (17%). Cutaneous AMLs are well-circumscribed, whitish-gray dermal tumors measuring 0.4-5 cm, generally smaller than their classic counterpart. They are histologically well circumscribed with an admixture of small to medium, thick-walled, muscular blood vessels, mature adipose tissue, and smooth muscle bundles in variable proportions, similar to classic AML (Figure 1). A fibrous pseudocapsule encloses the majority of cases, most likely as a stromal reaction to tumor growth. There are instances where atrophy or hyperplasia of the epidermis is visible. Unlike classic AML, there is no epithelioid variant in cutaneous AMLs; consequently, they do not display cellular atypia, necrosis, or mitosis (Figure 2).
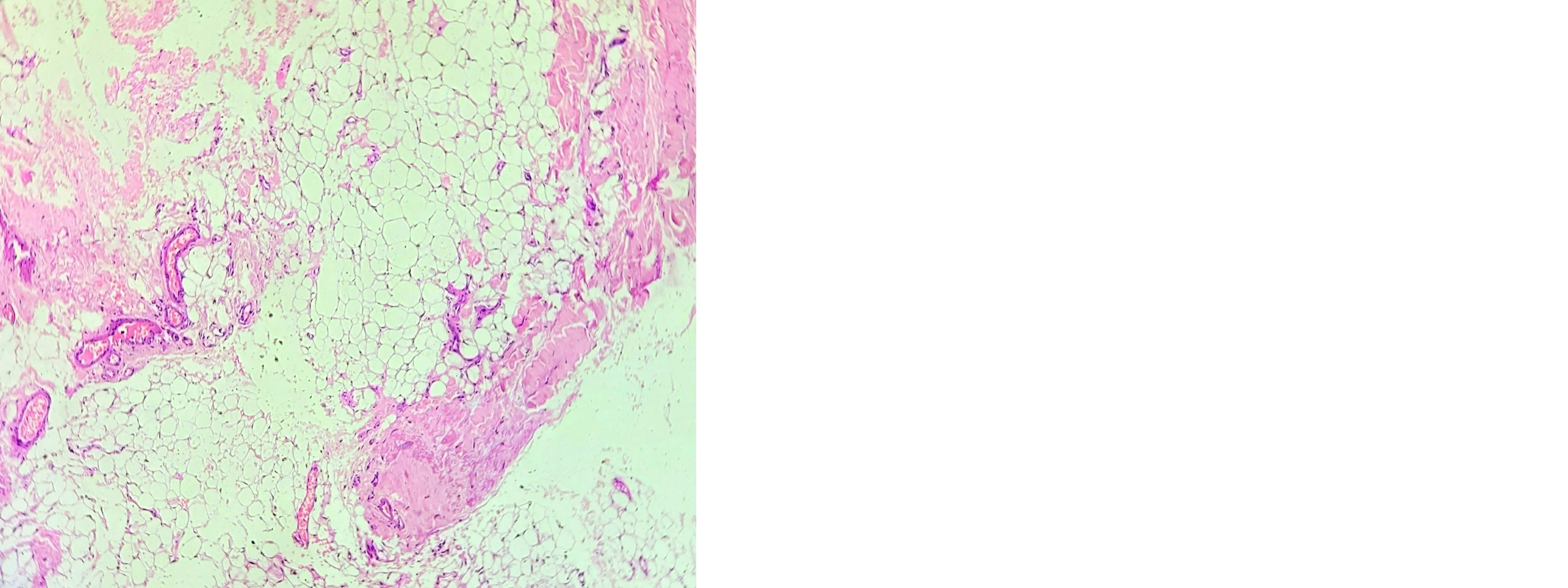
Figure 1: Hematoxylin-eosin-stained section demarcates variable-sized blood vessels, smooth muscle bundles, and mature fat tissue.
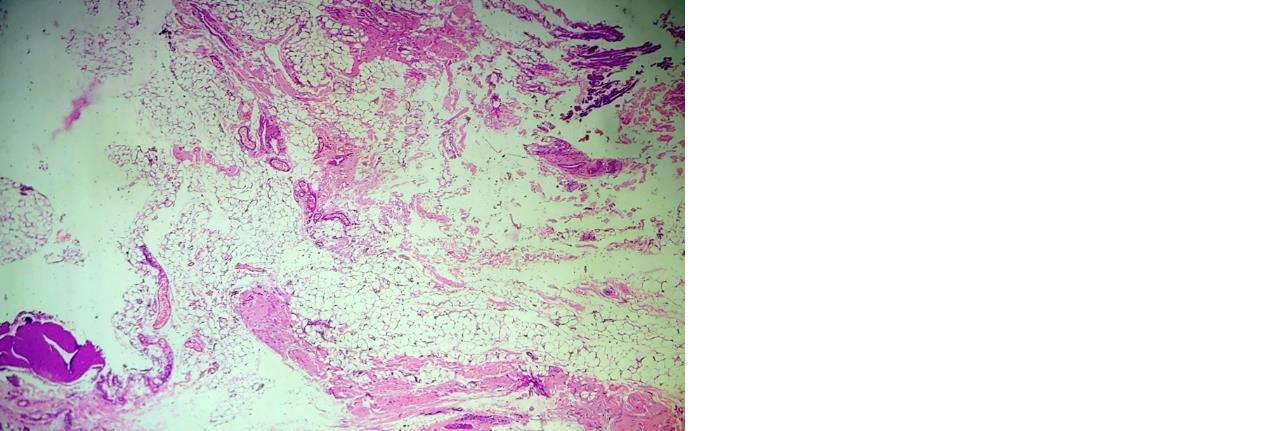
Figure 2: Haematoxylin-eosin-stained sections showing variable-sized blood vessels, smooth muscle bundles, and mature adipose tissue.
The irregular and diverse modifications observed in the smooth muscle component are indicative of pleomorphism. The fact that there were no epithelioid cells, no mitotic activity, necrosis, and the fact that the symptoms lasted for 15 years suggests that these findings are degenerative, like those seen in old schwannomas.
It is common for cutaneous AML to be positive for markers of smooth muscle, like SMA, Calponin, and Desmin. However, all cutaneous AMLs are negative for markers of melanocytes, like HMB-45, Melan-A, MART-1, and SOX-10 (Figure 3). Other frequently positive markers include S-100, Factor VIII, CD31, CD34, and FLI1.
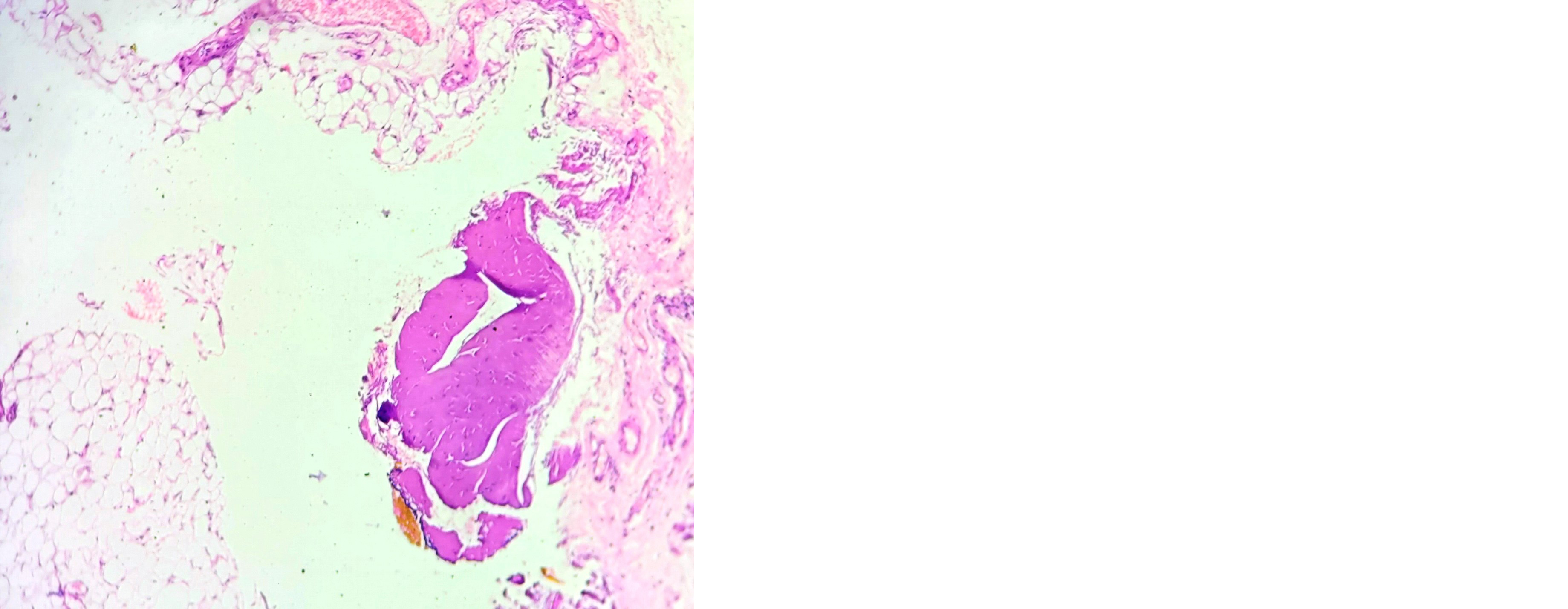
Figure 3: Haematoxylin-eosin-stained sections showing smooth muscle bundles and mature adipose tissue. Masson trichrome stained the muscular portions of the tumors bright red and the collagen Elastica van Gieson staining stained small arterioles within the lesions.
The recommended procedure for diagnosing and treating cutaneous AML is complete surgical excision, as it is typically a simple process to remove. Cutaneous AMLs are always benign and do not progress or recur even if the excision is incomplete. The most important differential diagnosis is classic AML in the skin since it is histologically identical. A few studies from the past five years reporting cutaneous AML are summarised in Table 1.
Table 1: Comparative analysis of few reported literature in last five years with present case study.
|
Parameters
|
Araujo et al [5]
|
Ditta et al [6]
|
Mannan et al [7]
|
Sanchez et al [8]
|
Kim YJ et al [9]
|
Present Case report
|
|
Year Published
|
2020
|
2021
|
2019
|
2022
|
2023
|
2024
|
|
Age
|
Two adults' age were not disclosed
|
2 years
|
36 years
|
35 years
|
43 years
|
59 years
|
|
Sex
|
Males
|
Boy
|
male
|
male
|
male
|
Male
|
|
Site
|
Earlobe
|
Eyelid
|
ear
|
Retro-auricular
|
Periorbital: Upper Eyelid
|
Umbilical
|
|
Surgery
|
Incomplete resection caused recurrence and others had complete resection
|
Complete resection
|
Complete resection
|
Complete resection
|
Complete resection
|
Complete resection
|
|
Tuberous sclerosis status
|
Negative
|
Present
|
Negative
|
Negative
|
Negative
|
Negative
|
|
Histopathology:
Triphasic criteria: blood vessels, smooth muscle cells, adipose tissue
|
present
|
Present
|
Present
|
Present
|
Present
|
Present
|
|
Immunohistochemistry
|
SMA-
HMB-45 -
|
SMA-diffuse +
HMB-45 Patchy positive
S- 100- immunonegative
|
Desmin +
Calponin+
HMB-45 –
Melan-A –
SOX10 –
Tyrosinase –
CD10 -
|
SMA +
HMB-45 –
Melan-A –
Tyrosinase -
|
SMA +
HMB-45 -
|
SMA+
HMB-45 -
|
Abbreviations: SMA- Smooth muscle actin: HMB -Human melanoma black
Conclusion
Angiomyolipoma is a rare benign tumour that can occur at extrarenal sites. The site was not a deciding factor in this particular case. Surgery plays a pertinent role in treating these cases however complete excision is important to prevent relapses. These varieties are rarely associated with tuberous sclerosis. Medical management in these scenarios is still under investigation.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Wang L, Leng B, Liu L. Angiomyolipoma of the nasal cavity: a distinct entity. Case report and literature review. Head Neck Pathol. 2021; 15:709–714.
[2] Kiran N, Ramanarasimhaiah R, Khan S, Mody K. Angiomyolipoma of Uterine Cervix: Report of a Rare Case. Cureus. 2023; 15:e38950.
[3] Thakur B, Hiwale KM. Intricacy in the Diagnosis of Retroperitoneal Angiomyolipoma: A Rare Case. Cureus. 2023; 15:e36357.
[4] Akçay H, Adak BM. Angiomyolipoma of the Hard Palate. Journal of Craniofacial Surgery. 2021; 32:e8–e9.
[5] Denadai R, Araujo K, Denadai R. Cutaneous angiomyolipoma of the ear: A rare diagnostic challenge. Indian Dermatol Online J. 2020; 11:226.
[6] Ditta LC, Zhang J, Bibars W, Bissler J. Cutaneous angiomyolipoma of the eyelid in a 2-year-old with tuberous sclerosis complex. J Neuro Ophthalmol. 2019; 41:e69–e70.
[7] Mannan AASR, Khandakar B, Yuan S. Cutaneous angiomyolipoma of the ear: case report and literature review. Am J Dermatopathol. 2019; 41:144–147.
[8] Sanchez NG, Romay AAÁ, Luna EM, Rodríguez ALP. Cutaneous Angiomyolipoma—A distinct entity that should be separated from classic angiomyolipoma: complete review of existing cases and defining fundamental features. JMIR Dermatol. 2022; 5:e40168.
[9] Kim YJ, Choi MH, Cheon JS, Choi WY. Periorbital cutaneous angiomyolipoma: A case report. Archives Craniofacial Surg. 2023; 24:83–86.