Full Text
Introduction
The increasing incidence of childhood obesity and its related morbidities, notably metabolic syndrome and non-alcoholic fatty liver disease (NAFLD), is a growing health concern worldwide. The prevalence of obesity is increasing at a much faster rate in lower and middle income countries (LMICs), as compared to Europe and North America, where it is reaching a high plateau [1]. The rising prevalence of obesity in a country like India, which is still fighting malnutrition, adds to the burden of chronic disease.
The World Health Organization (WHO) predicts that 1 in 5 women, and 1 in 7 men, will be obese with a BMI of > 30 kg/m2 by 2030. This amounts to over 1 billion people worldwide [1]. In India, a meta-analysis published in 2023 estimates the pooled prevalence of childhood obesity to be 8.4% and of overweight to be 12.4% [2].
Obesity often starts in childhood, and in India, parental or family concern about childhood obesity is low. An obese child is likely to become an obese adult, and therefore to live with a greater risk of chronic illness and noncommunicable diseases like cardiovascular disease, hypertension, diabetes, liver disease, and some cancers. As the prevalence of childhood obesity increases in India, so does the risk of early development and greater incidence of the above noncommunicable diseases [3]. Inexpensive, acceptable and easily available screening methods are an effective way to identify those obese children who are at risk.
There are many risk factors for cardiovascular disease (CVD). Abnormal lipids and obesity are among the most important [4]. A simple blood test can reveal an atherogenic lipid profile, and thus help to identify those individuals who are at high risk for CVD.
Non alcoholic fatty liver disease (NAFLD) is the commonest chronic liver disease in Asia [5]. Obesity is an important risk factor for development of NAFLD. Aspartate aminotransferase (AST) and Alanine aminotransferase (ALT) are the most commonly referenced biomarkers for liver damage in many liver diseases, including NAFLD. They are easy to obtain and low in cost, and therefore are of significant use as a screening tool.
We are seeing a rising number of obese children in recent years, even in clinics serving socioeconomically disadvantaged populations. As there are no studies describing the prevalence of dyslipidaemia or liver disease among obese children in Eastern India, we planned this study. Simple and inexpensive laboratory tests would help us screen individuals at risk and develop strategies for monitoring and prevention at an early stage.
Methods
This prospective, cross sectional, observational study was carried out in the Paediatric out patients department of our hospital, Ramakrishna Mission Seva Pratishthan, which is a tertiary care centre in Eastern India. The study period was from January 2023 to February 2024. Subjects were enrolled after obtaining approval from the Institutional Ethics Committee.
Children between 8-18 years who were referred for obesity included in this study. Those who had any other acute or chronic illness, or prolonged use of any medications, were excluded from the study. Written consent of the parent or caregiver, and verbal assent of the child, were obtained.
Sample size was calculated using Cochran’s Formula. Assuming the prevalence of obesity in India to be 8.4% [2], and allowing for an error of 6.9%, the sample size was calculated to be 62.
Sixty two obese children with no other acute or chronic illness were studied for the prevalence of dyslipidaemia and raised liver transaminases, AST and ALT. The IAP BMI charts for boys and girls (5-18 years) were used to confirm obesity. Only those individuals who were above adult equivalent of 27(Obesity) as per the BMI charts were enrolled [6].
Clinical examination included measurement of height, weight, blood pressure, and calculation of BMI. The children were clinically examined for any possible evidence of underlying disease as well. Laboratory analysis included estimation of serum triglyceride (TG), total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), and liver transaminases, AST and ALT.
Biochemical methods
Triglycerides, TC, and HDL were estimated by dry chemistry method, which is a colorimetric procedure on a slide. Wet Chemistry method was used for LDL, which uses colorimetry with a liquid reagent. VLDL is a derived value [VLDL = TC-(LDL +HDL)].
Definition of dyslipidemia
Lipid values in children vary by age and gender. As per the Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents [7), the following cutoffs were used to identify those individuals at high risk: i.e., TC : > 200mg/dl; LDL-C:> 130 mg/dl; Non-HDL-C: >145 mg/dl; TG:0 to 9 years - >100 mg/dl; 10 to 19 years- >130 mg/dl; HDL-C: < 40 mg/dl. Because the cutoffs for dyslipidemia vary by age , the subjects were divided into two groups: below 9 years, and 9 years and above.
Cutoffs for transaminases
There are no gender-specific cutoff data for ALT or AST published in India. Cutoffs used in the US are as follows: ALT >26mg/dl for boys, and >22mg/dl for girls. To screen for NAFLD, we used two times gender-specific ALT as per recommendations [8]: ALT >50mg/dl for boys, >44 mg/dl for girls.
AST has not previously been tested as a screening tool for NAFLD in children. Therefore, the cutoff value was decided as >46mg/dl, which was the reference range of our laboratory.
Statistical analysis
The data was recorded in an Excel spreadsheet. The software used for data analysis was MS-Excel/STATA 14. A p value of <0.05 was considered significant for analytical purposes.
Results
This study showed a significant correlation of BMI with triglycerides, total cholesterol, VLDL (Very low density lipoproteins), AST and non-HDL-C. Body mass Index is an easily calculated value in the OPD and this known correlation can help with some early counselling, even before any blood test reports are available. Children who feel well may often refuse a blood test).
Out of a total of 62 subjects, 37 (59.7%) were boys and 25 (40.3%) were girls. Among the boys, 35.14% (13 boys) were <9 years and 64.86% (24 boys) were >9 years. 20% of the girls (5 girls) were < 9 years and 80% (20 girls) were >9 years age. In total, 29.03% of all the subjects were 9 years or less and 70.97% were between the ages of 8-18 years (Figure 1).
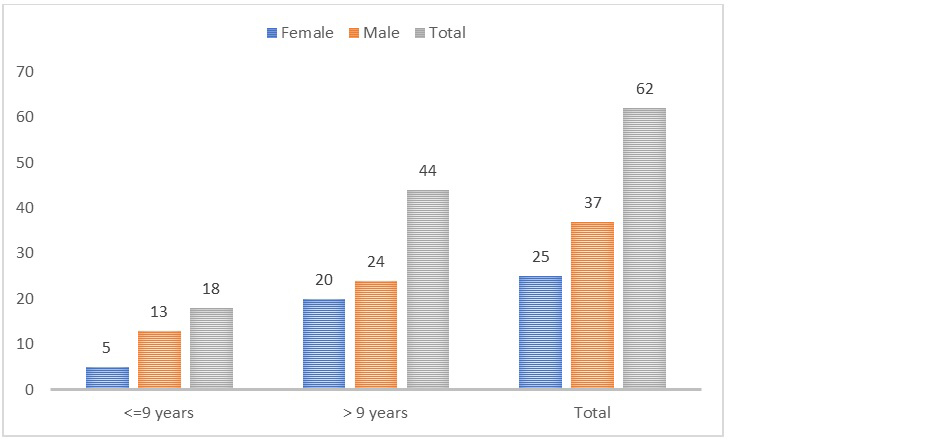
Figure 1: Gender distribution by age.
Dyslipidaemia was prevalent in 66.13%. 72% of the girls and 62.16% of the boys were found to be dyslipidaemic. However, this gender difference in prevalence was not statistically significant (Table 1).
Table 1: Prevalence of dyslipidaemia by gender.
|
|
Dyslipidaemia
|
Prevalence %
|
Value
|
|
No
|
Percentage
|
Yes
|
Percentage
|
|
Female
|
7
|
33.33%
|
18
|
43.90%
|
72.00%
|
Chi-square value: 0.644
|
|
Male
|
14
|
66.67%
|
23
|
56.10%
|
62.16%
|
p value: 0.422
|
|
Total
|
21
|
100.00%
|
41
|
100.00%
|
66.13%
|
|
On looking at the prevalence of dyslipidaemia by age, 66.67% of obese children < 9 years of age and 65.91% of those >9 years age had abnormal lipid profiles (Table 2). Again, the difference in prevalence by age was not statistically significant.
Table 2: Prevalence of dyslipidaemia by age.
|
|
Dyslipidaemia
|
Prevalence %
|
Values
|
|
No
|
Percentage
|
Yes
|
Percentage
|
|
<=9 years
|
6
|
28.57%
|
12
|
29.27%
|
66.67%
|
Chi-square value: 0.0032
|
|
> 9 years
|
15
|
71.43%
|
29
|
70.73%
|
65.91%
|
p value: 0.9543
|
Further analysis of the lipid profiles showed the following results (Table 3): 66.13% of the subjects had at least one abnormal lipid profile parameter (TG, HDL, or non-HDL-C). 50% had abnormal TG. 43.55% had an abnormally low HDL, and Non-HDL-C was high in 29.03%. 8.06% of the obese children had combined dyslipidaemia, with all three values abnormal (Figure 2). TG & HDL were both abnormal in 29.03%, and 11.29% had normal TG levels but abnormal HDL and non-HDL-C. In 24.19%, TG and non-HDL-C were raised, but HDL was normal.
Table 3: Lipid profiles.
|
Abnormal TG
|
31
|
50.00%
|
|
Abnormal HDL
|
27
|
43.55%
|
|
Abnormal Non-HDL-C
|
18
|
29.03%
|
|
All of the parameters are abnormal
|
5
|
8.06%
|
|
Both TG & HDL are abnormal
|
18
|
29.03%
|
|
Both HDL & Non-HDL-C are abnormal
|
7
|
11.29%
|
|
Both TG & Non-HDL-C are abnormal
|
15
|
24.19%
|
|
Either of TG, HDL or Non-HDL-C are abnormal
|
41
|
66.13%
|
|
Neither of TG, HDL or Non-HDL-C are abnormal
|
21
|
33.87%
|
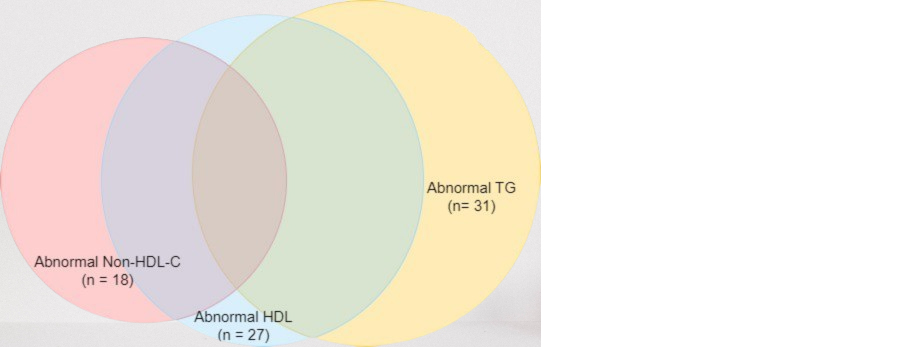
Figure 2: 8.06% (n=5) had combined dyslipidaemia.
The overall prevalence of transaminitis was 41.94%. 28% of girls had raised transaminase levels as compared to 51.35% boys (Table 4).
Table 4: Prevalence of transaminitis.
|
|
Raised ALT, AST
|
Prevalence %
|
Value
|
|
No
|
Percentage
|
Yes
|
Percentage
|
|
Female
|
18
|
50.00%
|
7
|
26.92%
|
28.00%
|
Chi-square value: 3.341
|
|
Male
|
18
|
50.00%
|
19
|
73.08%
|
51.35%
|
p value: 0.068
|
Both ALT and AST were raised in 30.65% and only ALT was raised in 40.32% (Table 5).
Table 5: Prevalence of raised transaminases.
|
AST raised
|
20
|
32.26%
|
|
ALT raised
|
25
|
40.32%
|
|
Both raised
|
19
|
30.65%
|
|
Neither raised
|
36
|
58.06%
|
|
Either AST or ALT is raised
|
26
|
41.94%
|
This study showed a significant correlation of BMI with triglycerides, total cholesterol, VLDL (Very low density lipoproteins), AST and non-HDL-C (Table 6).
Table 6: Correlation of BMI with other variables.
|
BMI
|
Overall
|
|
Correlation coefficient
|
p value
|
|
TG
|
0.3063
|
0.0155
|
|
TC
|
0.2913
|
0.0216
|
|
LDL
|
0.2116
|
0.0988
|
|
HDL
|
-0.0662
|
0.6092
|
|
VLDL
|
0.3104
|
0.0141
|
|
AST
|
0.2968
|
0.0192
|
|
ALT
|
0.139
|
0.2812
|
|
NON-HDLC
|
0.3146
|
0.0128
|
Discussion
In recent years, the rapidly increasing prevalence of childhood obesity and overweight have become a matter of serious concern. A study published in 2022, based on NFHS data, reported that the prevalence of overweight in under-fives has increased from 2.1% in 2015-16 to 3.4% in 2019-21 [9]. At more than 14.4 million obese children, India has the second highest number of obese children globally, second only to China [10].
In this study, 66.67% of obese children <9 years of age and 65.91% of those >9 years had abnormal lipid profiles. Obesity and associated cardiovascular risks are generally perceived by parents to be problems of adulthood and they think that there is enough time for course correction later. This might not be the case for the majority of obese children and adolescents. A study which tracked overweight status from childhood to young adulthood discovered that obese children and adolescents are likely to become obese adults [11]. If obesity in childhood tracks into adulthood, then the weight and dyslipidaemia of young children needs to be addressed urgently and not when they grow up.
Overall, the study showed dyslipidaemia in 66.13% of the subjects, where one or more of the lipid parameters (TG, HDL, non-HDL-C) was abnormal. All 3 combined, were abnormal in 8.06%.
In childhood, the predominant hyperlipidaemic pattern is characterised by elevated TG and non-HDL-C with reduced HDL-C. As described by Kavey [12], this is combined dyslipidaemia, occurring almost exclusively with obesity in children and seen in 30-60% of obese adolescents. There is an increased number of LDL particles and small, dense LDL along with a decrease in HDL and the number of large HDL particles. This is a highly atherogenic pattern and associated with evidence of atherosclerosis. The metabolic syndrome, NAFLD, visceral adiposity and insulin resistance are all associated with CD.
However, despite the serious risks, CD shows a good response to dietary and lifestyle interventions, which include weight loss and physical activity. Identifying these risk factors early and following management recommendations are critical in order to achieve a good outcome.
There was a high prevalence of raised serum transaminases among obese children in this study. Liver transaminases, AST and ALT, are commonly used markers of liver damage. Just like obesity and dyslipidaemia, NAFLD can be considered to be a pandemic disease. It is multifactorial but the increase in obesity and metabolic syndrome has led to increased prevalence of NAFLD. It is a serious liver disorder ranging from simple steatosis to hepatic inflammation, fibrosis, cirrhosis, even hepatocellular cancer.
The high prevalence of NAFLD makes it difficult to screen the population but a rational approach would be to screen individuals who are at high risk of NAFLD. Obese children fall into this category.
The diagnosis of NAFLD can be made by non-invasive means like a blood test for serum AST, ALT, other serum markers, imaging techniques like ultrasonography or MRI, and liver biopsy. Liver biopsy remains the gold standard for diagnosis but its invasive nature, cost and variability in sampling preclude its use in all patients suspected of NAFLD. Therefore, despite drawbacks, non-invasive methods may help to identify probable NAFLD and thereby reduce the number of patients needing a liver biopsy [13].
This study showed a significant positive correlation between BMI and triglycerides, total cholesterol, VLDL, non-HDL-C and AST. There are no similar studies on obese children from Eastern India but a study from Northern Mexico in 2016 [14] showed that even children as young as 2-10 years old with raised ALT had a higher prevalence of dyslipidaemia than those with normal ALT. Raised transaminase levels were associated with a high prevalence of combined dyslipidaemia. The AST/ALT ratio correlated with cardiometabolic risk factors of lipid profile. This raises the possibility of using AST/ALT as a screening test in the assessment of children with obesity and cardiometabolic risk.
Limitations: The data for this study was obtained from a tertiary care centre and may not accurately represent the situation in the community. A larger, multi-centre study , preferably including children and adolescents from the community, would provide more conclusive evidence.
Conclusion
Children with obesity have a high prevalence of dyslipidaemia and elevated transaminase levels, raising concerns about this obesity and metabolic risk tracking into adulthood and causing early onset of cardiovascular and liver disease. Simple, reliable and inexpensive screening tests which include anthropometry, lipid profile, and liver transaminase estimation, along with timely interventions to correct obesity are critical if we want a healthy population with a low prevalence of non-communicable diseases. Policy interventions which regulate the marketing and availability of inappropriate or harmful foods, and effective education about healthy lifestyles, are urgently needed.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Tim Lobstein TL. World Obesity Atlas, 2022.
[2] Singh S, Awasthi S, Kapoor V, Mishra P. Childhood obesity in India: A two-decade meta-analysis of prevalence and socioeconomic correlates. Clin Epidemiol Glob Health. 2023; 23:101390.
[3] El-Koofy NM, Anwar GM, El-Raziky MS, El-Hennawy AM, El-Mougy FM, et al. The association of metabolic syndrome, insulin resistance and non-alcoholic fatty liver disease in overweight/obese children. Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc. 2012; 18:44–49.
[4] Castelli WP. Lipids, risk factors and ischaemic heart disease. Atherosclerosis. 1996; 124:S1–S9.
[5] Seto WK, Yuen MF. Nonalcoholic fatty liver disease in Asia: emerging perspectives. J Gastroenterol. 2017; 52:164–174.
[6] Parekh BJ, Khadilkar V. Pediatrician-Friendly IAP Growth Charts for Children Aged 0-18 Years. Indian Pediatr. 2020; 57:997–998.
[7] Gujral J GJ. Pediatric dyslipidemia. In: StatPearls. Internet; 2023. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK585106/
[8] Vos MB, Abrams SH, Barlow SE, Caprio S, Daniels SR, et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr. 2017; 64:319–334.
[9] Saha J, Chouhan P, Ahmed F, Ghosh T, Mondal S, et al. Overweight/obesity prevalence among under-five children and risk factors in India: A cross-sectional study using the National Family Health Survey (2015–2016). Nutrients. 2022; 14:3621.
[10] The GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017; 377:13–27.
[11] Deshmukh-Taskar P, Nicklas TA, Morales M, Yang SJ, Zakeri I, et al. Tracking of overweight status from childhood to young adulthood: the Bogalusa Heart Study. Eur J Clin Nutr. 2006; 60:48–57.
[12] Kavey REW. Combined Dyslipidemia in children and adolescents: a Proposed New Management Approach. Curr Atheroscler Rep. 2023; 25:237–245.
[13] Lonardo A, Nascimbeni F, Maurantonio M, Marrazzo A, Rinaldi L, et al. Nonalcoholic fatty liver disease: Evolving paradigms: World J Gastroenterol. 2017; 23:6571–6592.
[14] Bibiloni MDM, Salas R, Nuñez GM, Villarreal JZ, Sureda A, et al. Relation between Liver Transaminases and Dyslipidaemia among 2-10 y.o. Northern Mexican Children. PLoS One. 2016; 11:e0155994.