Full Text
Introduction
Laryngoscopy and endotracheal intubation during induction of general anaesthesia produce strong nociceptive stimuli, which often result in profound stimulation of the sympathetic nervous system [1]. Because the upper airway reflexes protect the respiratory gas exchange surface from noxious substances, the nose, mouth, pharynx, larynx, trachea, and carina have sensory nerve endings and brisk motor responses abundantly. Afferent pathways for the cardiovascular responses to endotracheal intubation are initiated by the glossopharyngeal nerve when stimulation occurs superior to the anterior surface of the epiglottis and by the vagus nerve when stimulation occurs from the level of the posterior epiglottis down into the lower airway. In general, cardiovascular changes associated with intubation are transient and do not cause significant side effects. However, in patients with concomitant coronary artery disease, hypertension, or intracranial pathology, exaggerated hemodynamic parameters may cause myocardial ischemia or secondary brain damage. Many drugs are successfully used to suppress this stress response [2]. However, the administration of an additional drug may cause abnormal hemodynamic effects or may unnecessarily increase the depth of anesthesia. Therefore, non-pharmacological measure is preferred to reduce the response.
The extent of hemodynamic response depends on the type and depth of general anesthesia, the age of the patient, comorbidities like diabetes, cardiovascular diseases or other systemic diseases, and the drugs used [2]. This response also depends on the duration of laryngoscopy and intubation and the ease of the procedure [3, 4]. Therefore, achieving adequate neuromuscular blockade with neuromuscular blocking agents is extremely important from the point of view of decreasing the sympathetic response. Thus, assessment of complete neuromuscular blockade appears to be essential for proper timing of intubation. However, neuromuscular monitoring and precise timing are rarely used in clinical practice, and many anesthesiologists commence laryngoscopy based on clinical judgment after the normal onset time of the neuromuscular blocking agent used. A previous study showed that clinical judgment underestimated the time required for vecuronium to take effect, resulting in less favorable intubating condition [3-5]. Therefore, the aim of this study is to evaluate the monitoring of neuromuscular blockade in the prevention of hemodynamic fluctuations following laryngoscopy and tracheal intubation after administration of vecuronium in comparison with clinical evaluation of the time of laryngoscopy and tracheal intubation.
The objective of the study was to compare the hemodynamic response between clinical assessment and neuromuscular block monitoring guided tracheal intubation in patients undergoing general anaesthesia. The primary objective was to compare the intubation response using clinical parameters like heart rate, systolic BP, diastolic BP, and mean arterial pressure with train of four guided intubation and clinically guided intubation. The secondary objective was to study the onset of intubation with train of four guided intubation and compare with clinically guided intubation.
Materials and methods
This is a prospective, randomised, double blinded comparative clinical trial done in the Department of Anaesthesiology, Mysore Medical College and Research Institute, Mysore, K.R Hospital, Mysore during the period of December 2021 to July 2022. Institutional Ethical Committee approval obtained (I.E.C No. 24/2020). This study was done on patients posted for Elective Surgeries under General anaesthesia on 30 patients in each group. 60 patients were randomly divided into two groups of 30 each (Group C- Orotracheal intubation under clinical guidance and Group M- Orotracheal Intubation under neuromuscular monitor guidance) by computed generated randomization. p value less than 0.05 will be considered statistically significant.
All ASA grade I and grade II patients between 18-60 years age group were included in the study. Our study excluded All ASA grade III and IV patients, Patients with neuromuscular diseases, psychiatric illness, patients on antipsychotics, anxiolytics and antiepileptic drugs and obesity (BMI>30kg/m2) and sleep disorders.
Methodology
On the previous day of surgery, a thorough pre-anaesthetic examination of all the subjects in both the groups, with necessary basic investigations was done. Informed consent was obtained and Anaesthesia was induced with inj. Propofol. In Group C, endotracheal intubation was done following clinical assessment of neuromuscular blockade. In Group M, endotracheal intubation was done following neuromuscular block monitoring by TOF. In Group C, the timing of intubation was judged based on clinical assessment which started 1 min after the administration of muscle relaxant and at every 30 s thereafter by an experienced anaesthesiologist. The timing of laryngoscopy was judged on the basis of ease of ventilation, jaw and upper airway tone. In Group M, anaesthesiologist performed intubation after complete loss of all 4 responses to TOF stimulation that is TOF count zero. The endotracheal intubation was carried out with tubes of appropriate sizes. The time interval between the administration of neuromuscular blocking drugs to the time of tracheal intubation and cuff inflation was noted. Those patients who had oesophageal intubation were excluded from the study. Following that mechanical lung ventilation is performed using sevoflurane in an oxygen: Nitrous oxide (40:60) mixture. The primary outcome was hemodynamic changes in response to tracheal intubation. HR, SBP, DBP, MAP were recorded at
• T0 – before shifting the patient to OT table (baseline data)
• T1 – immediate after vecuronium administration
• T2 – after inflation of the cuff following intubation
• T3 – 1 min after intubation
• T4 – 3 min after intubation
• T5 – 5 min after intubation.
The secondary objectives included assessing the time between the administration of a neuromuscular blocking agent and endotracheal intubation (end of 5s inflation of the sealing cuff).
Results
The demographic data of the present study showed that the mean age in Group C was 45.27 years and in Group M was 47.20 years (p value = 0.649). Majority of the patients belonged to age group of 35-50 years (20/60; 33%). Majority of the patients were males (31/60) compared to females (29/60) with a male: female ratio of 1.06. Majority of the patients in Group C had ASA grade of 2 (24/30; 80%); majority in Group M also had ASA grade 2 (26/30; 87%) (p value= 0.488).
The heart rate levels in Group C and Group M were compared and shows that heart rate was significantly higher in Group C than Group M at inflation of cuff and at 1 min, 3 min, 5 min, following intubation compared to Group M with p value < 0.0001 (Table 1).
Table 1: Showing heart rate response to intubation.
|
Time
|
N
|
HR
|
p value
|
|
Neuromuscular monitor
|
Clinical
|
|
0
|
30
|
83±9.81
|
84.65±6.44
|
|
|
1
|
30
|
82.83±8.74
|
83.76±7.6
|
|
|
2
|
30
|
82.03±6.99
|
84.76±7.61
|
|
|
3
|
30
|
82.87±5.74
|
89±6.95
|
<0.001
|
|
4
|
30
|
83.37±5.08
|
87.4±8.24
|
<0.001
|
|
5
|
30
|
81.27±6.13
|
85.3±5.72
|
<0.001
|
|
6
|
30
|
80.1±5.59
|
84.2±5.82
|
<0.001
|
Systolic blood pressure in both Group C & Group M at baseline were recorded, at induction, at inflation of cuff and at 1 min, 3 min and 5 min following intubation. The mean SBP in Group C was 135.05±9.61, 129.11±9.52, 125.23±10.67, 121.43±12.19 at inflation of cuff, 1 min, 3 min 5 min following intubation respectively. The mean SBP in Group M was123.27±8.95, 122.53±10.52, 119.63±11.63 115.63±11.01 at inflation of cuff, 1 min, 3 min, 5 min following intubation respectively. This shows that SBP was significantly higher in Group C than Group M at inflation of cuff, and at 1 min, 3 min, 5 min following intubation compared to Group M with p value <0.0001 (Figure 1). The mean DBP in Group C was 92.97±6.63, 89.23±7.82, 87.93±7.09, 86.83±7.78 at inflation of cuff, 1 min, 3min 5 min following intubation respectively. The mean DBP in Group M was 85.73±8.74, 84.05±8.37, 83.13±8.86, 80.93±8.02 at inflation of cuff, 1 min, 3 min 5 min following intubation respectively. This shows that DBP was significantly higher in Group C than Group M at inflation of cuff, and at 1 min, 3 min, 5 min following intubation compared to Group M with p value <0.0001 (Figure 2).
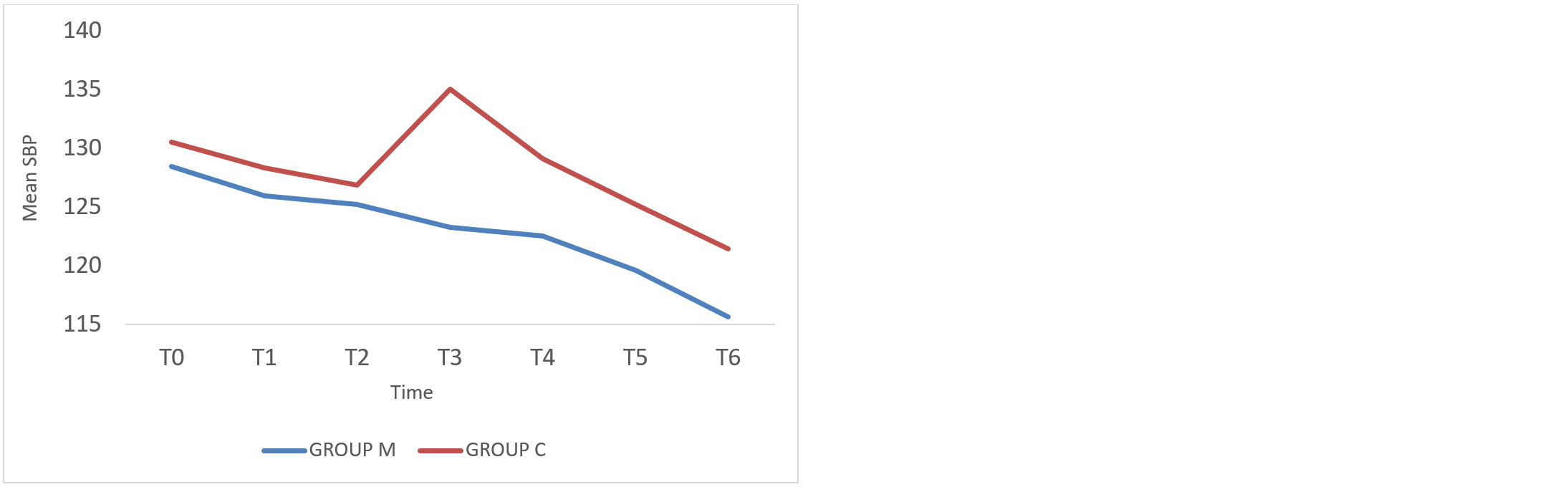
Figure 1: Showing systolic blood pressure response to intubation.
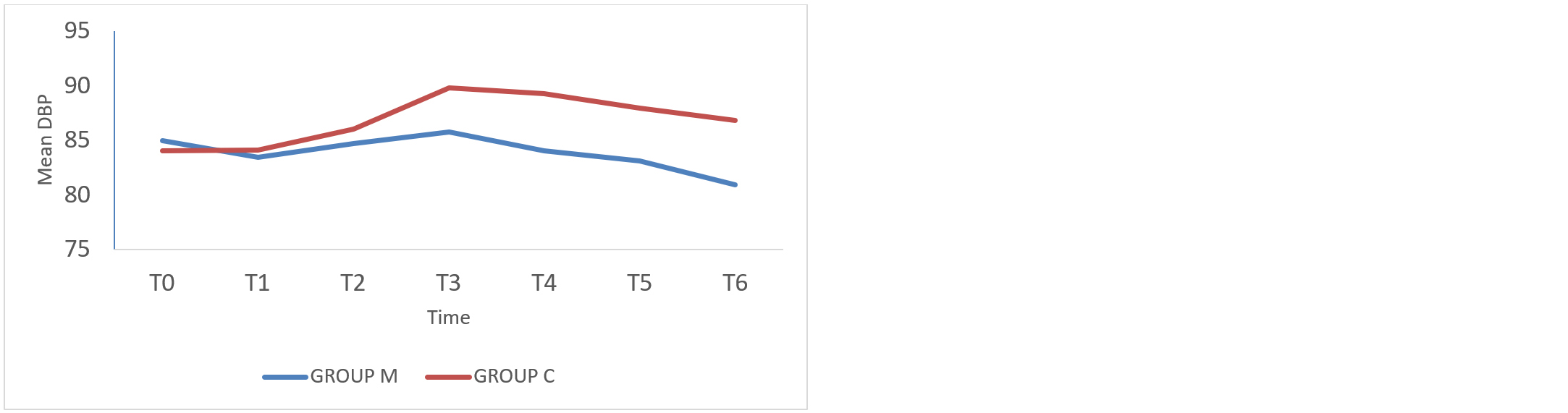
Figure 2: Showing diastolic blood pressure response to intubation.
The mean MAP in Group C was 100.87±6.02, 100.08±6.78, 99.17±6.9, 92.77±7.36 at inflation of cuff, 1min, 3min 5min following intubation, respectively. The mean MAP in Group M was 97.77±7.71, 96.75±6.88, 95.56±7.88, 93.34±7.37 at inflation of cuff, 1min, 3min, 5min following intubation respectively. This shows that MAP was significantly higher in Group C than Group M at inflation of cuff, and at 1min, 3min, 5min following intubation compared to Group M with p value <0.0001 (Table 2).
Table 2: Showing mean arterial pressure among the two groups.
|
Time
|
N
|
MAP
|
p value
|
|
Neuromuscular monitor
|
Clinical
|
|
0
|
30
|
97.77±8.28
|
98.53±6.4
|
|
|
1
|
30
|
97.27±7.99
|
99.87±6.49
|
|
|
2
|
30
|
97.43±7.14
|
99.97±7.7
|
|
|
3
|
30
|
97.77±7.71
|
100.87±6.02
|
<0.001
|
|
4
|
30
|
96.75±6.88
|
100.08±6.78
|
<0.001
|
|
5
|
30
|
95.56±7.88
|
99.17±6.9
|
<0.001
|
|
6
|
30
|
93.34±7.37
|
92.77±7.36
|
<0.001
|
The comparison of the mean time for intubation (seconds) in Group C and Group M was found to be 174.10± 10.67 and 385.17 ± 85.94 respectively. It shows the mean time for intubation was significantly longer in Group M than Group C.
Discussion
Direct laryngoscopy and endotracheal intubation following induction of anesthesia is almost always associated with hemodynamic stress response due to sympathoadrenal discharge. This sudden sympathoadrenal discharge is a potentially hazardous side effect of anesthesia technique. Sudden hypertension and increase in heart rate increased work load on heart and disturbs oxygen supply demand balance. It may present as rate and rhythm abnormalities, intracranial haemorrhage, organ dysfunctions of kidney and brain especially so in compromised patient like hypertensives, diabetics, coronary vascular disease, cerebrovascular disease, renal disease to name a few [6].
A variety of anesthetic drugs and techniques are available to control the hemodynamic response to laryngoscopy and intubation. The method or drug of choice depends on the many factors including urgency and length of the surgery, choice of anesthetic technique, route of administration, medical condition of the patient, and individual preference [9]. The possible solutions based on medications and techniques depend on the individual patient and the anesthesia care provider. Kovac et al reviewed the medications and techniques to guide the clinician in choosing the best method to control the hemodynamic response to laryngoscopy and endotracheal intubation [1].
However administration of an additional drug might cause adverse hemodynamic effect or might unnecessarily deepen the depth of anesthesia. Hence, a non-pharmacological measure to reduce the response is preferred. This response also depends on the duration of laryngoscopy and intubation as well as ease of procedure [2].
Shirbman et al also studied cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Arterial pressure, heart rate and plasma adrenaline and nor adrenaline concentrations were measured before and after induction after laryngoscopy and endotracheal intubation and they compared the hemodynamic response with and without intubation. There were significant and similar increase in blood pressure and circulating catecholamines concentrations following laryngoscopy with or without intubation. Intubation, however was associated with increase in heart rate which did not occur in laryngoscopy only group [8]. This they explained as due to the balanced stimulation of both vagal and cardioaccelerator fibres by laryngoscopy but intubation lacked vagal stimulation [8]. Previous studies showed that the hemodynamic response to laryngoscopy and intubation will also depend on the duration of laryngoscopy and intubation as well as the ease of procedure [2].
In this study, adequate neuromuscular blockade was ensured by neuromuscular monitor by observing response to TOF stimulation. In the neuromuscular monitoring Group (M), intubation was performed when there was complete loss of all 4 responses to TOF stimulation. . Those patients intubated by clinical judgment showed higher mean values of mean arterial pressure and HR during and after intubation in comparison to the patients who were intubated under guidance of neuromuscular monitoring (P < 0.05). It has been observed that patients with incomplete neuromuscular block experience a more intense hemodynamic response during laryngoscopy and intubation due to increased nociceptive stimulation.
Witkowska et al concluded that neuromuscular block monitoring following neuromuscular blockade prolongs the endotracheal intubation time, improves intubation conditions and minimises cardiovascular responses. In their study, 162.3 ± 35 s (mean ± SD) is the mean time for intubation in patients under clinical monitoring group and 339.3 ± 73.7 s (mean ± SD) is the mean time for intubation in patients under neuromuscular monitoring group [9].
The use of vecuronium as a muscle relaxant led to clinical judgment underestimating the time needed for adequate onset of action, resulting in suboptimal intubating conditions. Monitoring neuromuscular block also prolonged the time between vecuronium administration and intubation. Additionally, there is a substantial variation in intubation times among patients in the neuromuscular monitoring group compared to the conventional clinical based group. Control group, we intubated the patients following clinical judgment, this similarity in intubation time in this group may be due to our habits in day-to-day practice neuromuscular block in our study [10].
Adductor pollicis muscle was chosen to monitor the neuromuscular block in our study. In study by Haller et al Curarisation time of the OO (Orbicularis oculi) was shorter (110 +/- 4.9 sec) than that of the AP (Adductor pollicis) (144 +/- 5.5 sec; P < 0.0001). Intubation conditions were excellent in 95% and good in 5% of the patients in the AP group whereas in the OO group only 65% of the patients had excellent and 20% good intubation conditions (P < 0.05). They concluded that monitoring neuro-muscular activity of the AP using TOF to determine the appropriate tracheal intubation time and conditions in patients paralysed with rocurorium is more clinically relevant than monitoring the OO muscle [11]. The adductor pollicis muscle is chosen for monitoring in this study because it helps reduce the hemodynamic surge and is easier to monitor as a peripheral muscle.
In our study, in the clinical group, intubation was tried after an average of 174 s after vecuronium administration and in the neuromuscular monitoring group, where intubation was tried after an average of 385 s of vecuronium administration. Hemodynamic changes were less in Group M compared to Group C.
It is rare for anesthesiologists to use neuromuscular monitoring during endotracheal intubation. Typically, it is used for muscle relaxation monitoring during surgery and to detect any residual paralysis afterwards. More research on this topic is needed.
Conclusion
Neuromuscular block monitoring of adductor pollicis muscle ensured complete laryngeal muscle paralysis thus attenuate the haemodynamic responses to laryngoscopy and tracheal intubation significantly as compared to conventional clinical assessment method which purely depends on time of action of the drug used.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996; 8:63–79.
[2] Angelard B, Debry C, Planquart X, Dubos S, Dominici L, et al. Difficult intubations. A prospective study. Ann Otolaryngol Chir Cervicofac. 1991; 108:241–243.
[3] Soltesz S, Stark C, Noé KG, Anapolski M, Mencke T. Monitoring recovery from rocuronium-induced neuromuscular block using acceleromyography at the trapezius versus the adductor pollicis muscle: an observational trial. Can J Anaesth. 2016; 63:709–717.
[4] Jung W, Hwang M, Won YJ, Lim BG, Kong MH, et al. Comparison of clinical validation of acceleromyography and electromyography in children who were administered rocuronium during general anesthesia: a prospective double-blinded randomized study. Korean J Anesthesiol. 2016; 69:21–26.
[5] Parasa M, Vemuri NN, Shaik MS. Comparison of equipotent doses of rocuronium and vecuronium. Anesth Essays Res. 2015; 9:88–91.
[6] Singh G, Kaur H, Aggarwal S, Sharda G, Singh A, et al. Intravenous dexmedetomidine vs lignocaine in attenuating the hemodynamic responds during a laryngoscopy and endotracheal intubation : a randomized double blind study. Anesth Pain Intens care. 2017; 21:181–186.
[7] Pingle S, Sharma P, Dhumane P, Raipure A, Sharma A. Comparison of efficacy of lignocaine 1.5mg/kg & dexmedetomidine 1mcg/kg in attenuating hewmodynamic response to laryngoscopy and intubation. Int J Med. 2019; 7:339–347.
[8] Shirbman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine response to laryngoscopy with ir without intubation. Br J Anesth.1987; 59:295–299.
[9] Witkowska M, Karwacki Z, Wierzchowska J, Bukowski P. Monitorowanie Neuromuscular block monitoring for optimisation of conditions for endotracheal intubation. Anestezjol Intens Ter. 2009; 41:140–144.
[10] Carroll MT, Mirakhur RK, Lowry DW, McCourt KC, Kerr C. Neuromuscular blocking effects and train-of-four fade with cisatracurium: Comparison with other nondepolarising relaxants. Anaesthesia. 1998; 53:1169–1173.
[11] Haller G, Gardaz JP, Bissonnette B. Assessment of intubation time and conditions under the influence of rocuronium. Can J Anaesth. 1998; 45:312–316.