Orginal Research
2024
December
Volume : 12
Issue : 4
Evaluation of home based insulin therapy among pediatric patients with type I diabetes mellitus - A prospective analytical study
Soundararajan N, Thangavel A, Vidjeadevan D, Vijayaraghavan A
Pdf Page Numbers :- 304-309
Soundararajan N1,*, Thangavel A1, Vidjeadevan D1 and Annamalai Vijayaraghavan2
1Department of Paediatrics, KAPV Government Medical College, Trichy, Tamil Nadu 620001, India
2Department of Paediatrics, Metha Hospital, Chetpet, Chennai, Tamil Nadu 6000031, India
*Corresponding author: Dr. Soundararajan N, Department of Paediatrics, KAPV Government Medical College, Trichy, Tamil Nadu 620001, India. Email: dr.sound77@gmail.com
Received 2 July 2024; Revised 31 August 2024; Accepted 4 September 2024; Published 10 September 2024
Citation: Soundararajan N, Thangavel A, Vidjeadevan D, Vijayaraghavan A. Evaluation of home based insulin therapy among pediatric patients with type I diabetes mellitus - A prospective analytical study. J Med Sci Res. 2024; 12(4):304-309. DOI: http://dx.doi.org/10.17727/JMSR.2024/12-57
Copyright: © 2024 Soundararajan N et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Home based insulin therapy is one of the major challenges faced by the Type I diabetes mellitus (T1DM) patients with regards to the injection technique and correct dosing. The study aimed to assess the home based insulin therapy and its complications and to evaluate the impact of counselling on home based insulin therapy among Type I diabetes mellitus patients.
Methodology: A prospective analytical study was conducted at Institution of Child Health, Egmore for a period of one year. Children of age less than 15 years and are newly diagnosed with type I diabetes or recently diagnosed diabetes of less than 18 months duration were included as our study subjects. A non-random quota sampling technique was followed for sample calculation and based on that 85 children satisfying our inclusion and exclusion criteria were selected as our study sample.
Results: The demographic details shows that the mean age among males was 10.2 ± 3.2 and for females it was 8.9 ± 2.8 and the male: female ratio was 0.88: 1. It was observed among the study subjects that there was a regular improvement in their knowledge and practice over a period of time, during each visit the number of care givers with correct knowledge and practice were increasing starting from base level assessment to third follow-up visit and it was found to be statistically significant (p<.001).
Conclusion: The present study has proven that repeated education and proper training given to the care providers of Type I DM patients plays a major role in control of their diabetic status as well as preventing them from developing injection site complications.
Keywords: insulin injection technique; care providers; glycemic control
Full Text
Introduction
Type 1 diabetes mellitus (T1DM) is one of the leading causes of chronic ailment among the pediatric age group population. With the increasing prevalence of Type I DM more than half of them are living in developing nations, with India being home to an estimated(to be deleted) of more than 1 lakh children with T1DM [1]. The recent report from International Diabetes Federation (IDF), published in 2017 showed an estimate of 1.11million children and adolescents aged <20 years have type 1 diabetes, with 132,600 new cases being diagnosed annually [2]. Type 1 diabetes mellitus accounts for 5%–10% of all cases of diabetes. T1DM is a disease of concern as it has serious short term and long term implications. The incidence of T1DM is increasing by 3% every year, which leads to 75,000 new cases of T1DM every year [3]. Along with the increase in the incidence and the enhanced access to insulin, the survival rates have improved which would invariably lead to a higher prevalence of type I DM in the near future [4]. In India diabetes registry is not maintained and so the exact data on prevalence of type I DM is not available but based on different studies done at various states in India the prevalence rate was ranging between 3.5 – 5 /100,000 population and this was found to be higher than that reported from many other Asian countries [5].
Insulin is the main stay of treatment for Type I DM apart from diet and physical activity. Most of the time the physician’s advice towards the glycemic control was mainly on adjusting the dosage of insulin and a very little time was spent on improving Injection Technique (IT) [6]. Studies have proven that following a correct and proper injection technique could very much help in reducing the insulin dosage for patients with type I DM [6, 7]. As most of the victims for type I DM are children and the insulin providers for them would be either their parents or guardians for whom proper health education related to the technique of giving insulin injection should be given and it should be reinforced during every visit. Studies done earlier had shown that the following factors should be addressed in the education of giving insulin injection they are, injection site rotation, rolling to resuspend the insulin, and avoiding air bubbles, mixing of insulin, applying different colour codes for different types of insulin, refrigerating the insulin at appropriate temperature and recapping the needle after the injection [7-9]. Challenges relating to the poor treatment outcomes among children and adolescents with type 1 diabetes includes non-compliances and nocturnal hypoglycemic episodes, and a very close parental/guardian supervision is very much needed [8, 9]. However, improved and novel technologies including the use of insulin pens, insulin pumps, sensor-augumented pumps (SAPs) and artificial pancreas system improve the safety, effectiveness, and adherence to insulin regimen among children and adolescents with type 1 diabetes [10-12]. But cost is the major factor in utilizing these advanced technologies, so for developing countries like India proper education on giving insulin injection to the care givers is the need of the hour for effective glycemic control among Type I diabetes mellitus [13]. In India as such not many studies have been conducted to evaluate the insulin therapy and its complications, few studies that were conducted are on type II diabetes patients receiving insulin [14-16].
The present study aimed to assess the home based insulin therapy and its complications and to evaluate the impact of counselling on home based insulin therapy among Type I diabetes mellitus patients.
Methodology
A prospective analytical study was conducted at Institution of Child Health, Egmore for a period of one year from June 2021 to December 2022. The study was started after getting approval from the institutional ethics committee.
Children of age less than 15 years and are newly diagnosed with type I diabetes or recently diagnosed diabetes of less than 18 months duration were included as our study subjects. Children with congenital deformities and diabetes with other co-morbidities were excluded from the study. A non-random quota sampling (purposive sampling - sample size was fixed based on the time duration) technique was followed for sample calculation and based on that 85 children satisfying our inclusion and exclusion criteria were selected as our study sample.
Informed consent was obtained from either of their parents or guardians of all the children. A semi-structured questionnaire was designed to obtain the demographic data and the knowledge, attitude and practice regarding the dosing and technique followed for giving insulin to the children by the care givers. Three counselling sessions each of 20 minutes duration were scheduled and conducted by the investigator at an interval of 2 months for the care givers of the children with Type I diabetes, the following areas were covered in the counselling session by using audio-visual aid: Loading of insulin; injection technique; site rotation; disposal of syringe; looking for complications at the injection site; regular monitoring of the blood glucose levels.
The care givers of the children were provided with glucometer with strips, insulin cartridge and syringe, they were instructed to measure the fasting and post-prandial blood sugar levels. All children were followed for a minimum of 3 visits at an interval of 3 months. During each visit the care givers were enquired regarding the home based insulin treatment and the injection procedure was observed by the investigator and in case of any error it was recorded and corrected. HbA1C levels were assessed during each visit.
All data were entered and analysed using SPSS version 24. Mean and SD were calculated for all parametric variables and percentage was derived for frequency variables. Chi-square test was used to derive the statistical inference for the parameters assessed before and after counselling, considering P<.05 as statistically significant.
Results
The present study was conducted to evaluate the home based insulin therapy among 85 children with Type I diabetes mellitus. Among the 85 children majority were in the age group between 5 and 9 years with minimum age of 4 years and maximum age was 12 years, the mean age group among the study subjects was 10.2 years among male children and 8.9 years among female children. Male and female children were almost equal in number (Table 1).
Table 1: Age and gender wise distribution of the study subjects.
|
Age group
|
Male
|
Female
|
Total
|
|
<5 years
|
3 (7.5%)
|
5 (11.1%)
|
8
|
|
5 – 9 years
|
23 (57.5%)
|
31 (68.8%)
|
54
|
|
10 – 12 years
|
14 (35%)
|
9 (20%)
|
23
|
|
Total
|
40 (100%)
|
45 (100%)
|
85
|
|
Mean ± SD
|
10.2 ± 3.2
|
8.9 ± 2.8
|
|
The educational status of the care givers of diabetes children has a direct impact on the knowledge of home based insulin therapy in the management of diabetic children and so the educational status was assessed and it was found that 36% of them were not literate and 54% of them were educated up to high school level (Figure 1). Among our study subjects majority of the children were suffering from type I diabetes mellitus for more than 1 year (64.7%) and only for 2 children the duration of the illness was less than 6 months and the mean duration was found to be 13.5 months (Table 2).
Table 2: Distribution of the study subjects based on the duration of illness.
|
Duration of illness
|
Frequency
|
Percentage
|
Mean ± SD
|
|
<6 months
|
2
|
2.3%
|
13.5 ± 5.8
|
|
6 – 12 months
|
28
|
32.9%
|
|
12 – 18 months
|
55
|
64.7%
|
|
Total
|
85
|
100%
|
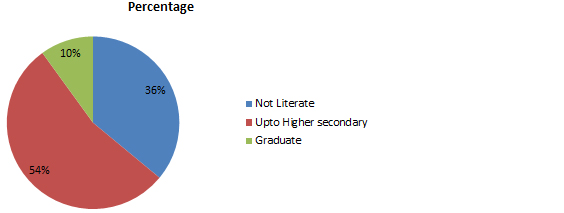
Figure 1: Educational Status of the care takers.
Initially the base level knowledge related to home based insulin administration was assessed among the care givers of the children. Majority of the care givers were the mothers of the children (94%). Among the various factors the base level knowledge was high for loading of insulin (91%) and limb rotation (87%), and the knowledge was poor for disposal of syringe (3.5%) and for cleaning of pre-injection site (12.9%). With this base level assessment all the care givers were counseled on regular basis using audio and video illustrations. It was observed among the study subjects that there was a gradual improvement in their knowledge and practice over a period of time, during each visit the number of care givers with correct knowledge and practice were increasing starting from base level assessment to third follow-up visit and it was found to be statistically significant (p<.001) (Table 3). The knowledge and practice level were more than 85% for almost all the factors related to home based insulin therapy except for disposal of insulin syringe (74%) and knowledge on site related complications (80%).
Table 3: Factors influencing the diabetic status in home based insulin therapy at base level and after repeated counselling.
|
Variables
|
Base level
|
First follow-up
|
Second follow-up
|
Third follow-up
|
p value
|
|
Loading of insulin correctly
|
78 (91.7%)
|
82 (96.4%)
|
84 (98.8%)
|
85 (100%)
|
<.001
|
|
Accuracy of insulin dose maintained
|
35 (41.1%)
|
46 (54.1%)
|
67 (78.8%)
|
74 (87%)
|
<.0001
|
|
Pre-injection site cleaning
|
11 (12.9%)
|
60 (70.5%)
|
82 (9.4%)
|
85 (100%)
|
<.0001
|
|
Skin pinch done correctly
|
44 (51.7%)
|
49 (57.6%)
|
65 (76.4%)
|
80 (94.1%)
|
<.0001
|
|
Correct position of needle angle
|
37 (43.5%)
|
49 (57.6%)
|
61 (71.7%)
|
76 (89.4%)
|
<.01
|
|
Limb rotation
|
74 (87%)
|
83 (97.6%)
|
85 (100%)
|
85 (100%)
|
<.01
|
|
Site rotation
|
52 (61.1%)
|
69 (81.1%)
|
81 (95.2%)
|
83 (97.6%)
|
<.001
|
|
Correct knowledge on site related complications
|
35 (41.1%)
|
49 (57.6%)
|
57 (67%)
|
68 (80%)
|
<.001
|
|
Disposal of syringe
|
3 (3.5%)
|
30 (35.2%)
|
45 (52.9%)
|
63 (74.1%)
|
<.0001
|
Initially, Self Monitoring of Blood Glucose (SMBG) was done by majority of the care givers on their diabetic children on monthly basis and by repeated counselling SMBG was performed weekly once by almost all care givers at the third follow-up visit (p<.001). Similarly the mean HbA1C levels was significantly improved during each follow-up visit compared to the base level and this difference in the improvement of HbA1C levels was found to be statistically significant (p<.001) (Table 4).
Table 4: Comparison of HbA1c and SMBG at base level and during regular follow-up.
|
Variables
|
Base level
|
First follow-up
|
Second follow-up
|
Third follow-up
|
p value
|
|
HbA1C (<8gms%)
Mean ± SD
|
31 (36.4%)
10.1 ± 1.87
|
43 (50.5%)
9.7 ± 1.74
|
58 (68.2%)
8.2 ± 1.34
|
71 (83.5%)
7.6 ± 1.12
|
<.001
|
|
SMBG done regularly at weekly once
|
36 (42.3%)
|
49 (57.6%)
|
76 (89.4%)
|
85 (100%)
|
<.0001
|
Discussion
In today’s world with rapid urbanization and industrialization the incidence of type 1 diabetes mellitus is increasing worldwide and more so among younger children. Unfortunately, as such in India we have a very little information about the incidence of type 1 diabetes in children but no studies were conducted to assess the home based insulin management among type I diabetes patients. Recent studies have emphasized the importance of strict glycemic control in preventing and delaying the chronic micro vascular complications in type I diabetes mellitus [14, 15]. In developing countries like India there are only few paediatricians and very few diabetes nurse educators who were properly trained in the management of type 1 diabetes. Home based insulin therapy given by the care takers of the children plays a pivotal role in the management of type I diabetes among children and so this study was designed to evaluate the prevailing issues in home based insulin therapy and the effect of counselling among the care takers of type 1 diabetic children.
In the present study the predominant age group of the study subjects was found to be between 5 and 10 years and female gender were slightly more than the male gender and most of the studies done earlier on Type I diabetes mellitus have shown the similar finding in the age group affected and both the gender were shown to be equally affected [16-18]. The major challenge faced by the type I diabetes patients is the regular intake of insulin, which would cause them the fear of pain, improper dosing and the needle site complications finally ending up in poor glycemic control. So the only cost effective tool available to address this issue is the regular education to the care givers of type I diabetes patients.
Holding the skin pinch correctly is an important parameter, as it determines the absorption of insulin and the pain experienced by the patients. A recent study done in India highlighted that the risk of i.m. injections are low when the skin pinch is done correctly and a 4mm size needle being used for delivering the insulin [19, 20]. In our study only 52% of the care givers did the skin pinch currently initially but after repeated counselling it was increased to 94%.
Vardar and Kizilci in their study through logistic regression analysis found out three independent risk factors for development of lipohypertrophy, they were prolonged insulin usage, failure of limb and site rotation and reuse of needles [21]. In our study the knowledge for the care givers related to limb and site rotation was 87% and 61% during the start of the study which was later improved to 100% and 97% at the end of three counselling sessions.
Earlier study had shown that audio-visual tools could be used to fill the gaps in the training of patients or the care givers on insulin injection skills [22-24]. Multimedia due to its unique characteristics it stimulates the learning interest among patients/care givers and helps to enhance their memory through images, text, and sound [25-29]. A recent study done in China by Cheng et al, where he used videos to guide training on insulin injection and found that this intervention had provided timely error correction among diabetic patients [30]. Another Turkish study by Celik et al used cell phone text messages to instruct diabetic patients on using insulin pens correctly [31]. These measures have found to improve the understanding and knowledge of the patients /care givers of diabetes and thereby it increased the injection skills among them.
In the present study less than 15% of the study subjects had the habit of cleaning the injection site before giving insulin before giving counselling which was gradually improved to 100% after the third counselling session. The studies done in Bangladesh and Nigeria showed a only 50 to 60% of the diabetes patients had the habit of cleaning the injection site but it was only a onetime assessment and post- counselling evaluation was not done [29, 30].
Systematic intra-site and inter-site rotation helps to maintain healthy injection sites, promotes good amount of insulin absorption and thereby reduces the chance of lipohypertrophy. Most of the participants in the present study used multiple sites for injections and majority of them had followed limb rotation (87%) and site rotation (61%) even before the counselling session and after three session of counselling almost all of them regularly practised both limb and site rotation and it was much better than the studies previously done in India, Bangladesh and Nigeria [28-30].
It is very important to provide education regarding insulin injection whenever a patient is prescribed with insulin, and such education should be repeated at regular intervals for better treatment outcomes. Patients in the present study received such education at the beginning after assessing their initial level of awareness and practice of insulin treatment, and regularly once in 2 months. But majority of the studies done earlier the education on insulin injection was given only at the beginning and that was not repeated periodically. Further it was mentioned that the lack of repeated education is the reflection of the current poor injection practice among their study population [31, 32]. Guidelines have made a strong recommendation for checking the injection sites at least yearly once, and more frequently for patients who are at risk of developing lipohypertrophy. Unfortunately, for more than 50% of our study subjects the treating physicians had never checked the injection site regularly and the situation is similar or worse in the studies done earlier [33].
There were few limitations in the present study. The sample size was not large, as we need regular follow up and repeated counselling for the care takers of Type I DM patients and so the sample size was restricted to 85. As not many studies have been conducted earlier to assess the insulin injection practices among the care takers of Type I DM, most of the studies that were conducted related to insulin injection practices were among the type II DM patients and so comparing our results with the previously conducted studies were very minimal.
Conclusion
Most of the care takers of type I DM patients were not following the ideal insulin injection practice during the start of the study but the practices improved significantly over a period of time after conducting repeated counselling and training sessions for the care takers. The complication of insulin injection site such as lipohypertrophy was not that high among our subjects. Our study had proven that repeated education and proper training given to the care providers of Type I DM patients plays a major role in control of their diabetic status as well as preventing them from developing injection site complications. So, apart from counselling the diabetes patients on diet and physical activity it is much more important to regularly counsel and train the diabetes patients or the care takers on insulin injection technique to achieve the glycemic control and prevent them from complications.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Kumar KM, Azad K, Zabeen B, Kalra S. Type 1 diabetes in children: Fighting for a place under the sun. Indian J Endocrinol Metab. 2012; Suppl 1:S1–S3.
[2] Kumar KMP. Incidence trends for childhood type 1 diabetes in India. Indian J Endocr Metab. 2015; 19:34–35.
[3] Ramachandran A, Snehalatha C, Krishnaswamy CV. Incidence of IDDM in children in urban population in southern India. Madras IDDM Registry Group Madras, South India. Diabetes Res Clin Pract. 1996; 34:79–82.
[4] Das AK. Type 1 diabetes in India: Overall insights. Indian J Endocr Metab. 2015; 19:31–33.
[5] Kumar P, Krishna P, Reddy SC, Gurappa M, Aravind SR, et al. Incidence of type 1 diabetes mellitus and associated complications among children and young adults: Results from Karnataka Diabetes Registry 1995 2008. J Indian Med Assoc. 2008; 106:708–711.
[6] Ji LN, Guo XH, Huang J. Chinese guideline for diabetic injection technology. Chin J Diabetes Mellitus. 2017; 9:79–105.
[7] Davel H, Berg GI, Allie R. Injection Technique Working Group of the Diabetes Education Society of South Africa (DESSA) Injection technique guidelines for diabetes: sharp and to the point. JEMDSA. 2014;19:8.
[8] Russell SJ, Hillard MA, Balliro C. Day and night glycaemic control with a bionic pancreas versus conventional insulin pump therapy in preadolescent children with type 1 diabetes: a randomised crossover trial. Lancet Diabetes Endocrinol. 2016; 4:233–243.
[9] Cemeroglu AP, Can A, Davis AT, Ozlam, Lora K, et al. Fear of needles in children with type 1 diabetes mellitus on multiple daily injections and continuous subcutaneous insulin infusion. Endocr Pract. 2015; 21:46–53.
[10] Sherr JL, Hermann JM, Campbell F, Nicole C, Sabine E, et al. Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control. comparison of results from three large, transatlantic paediatric registries. Diabetologia. 2016; 59:87–91.
[11] Smalley E. Medtronic automated insulin delivery device gets FDA nod. Nat Biotechnol. 2016; 34:1220.
[12] Szypowska A, Schwandt A, Svensson J, Shlomit S, Roque C, et al. Insulin pump therapy in children with type 1 diabetes: analysis of data from the SWEET registry. Pediatr Diabetes. 2016; 17:38–45.
[13] Hanas R, de Beaufort C, Hoey H. Insulin delivery by injection in children and adolescents with diabetes. Pediatr Diabetes. 2011; 12:518–526.
[14] Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The diabetes control and complications trial research group. N Engl J Med. 1993; 329:977–986.
[15] Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ et al. Resistance to insulin therapy among patients and providers: Results of the cross-national diabetes attitudes, wishes, and needs (DAWN) study. Diabetes Care. 2005; 28:2673–2679.
[16] Wangnoo SK, Maji D, Das AK, Rao PV. Barriers and solutions to diabetes management: An Indian perspective. Indian J Endocrinol Metab. 2013; 17:594–601.
[17] Patel A, MacMahon S, Chalmers J, Neal B, Billot L et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008; 358:2560–2572.
[18] Vasudevan AR, Burns A, Fonseca VA. The effectiveness of intensive glycemic control for the prevention of vascular complications in diabetes mellitus. Treat Endocrinol. 2006; 5:273–286.
[19] Rewers M, Norris J, Dabelea D. Epidemiology of type 1 diabetes mellitus. Adv Exp Med Biol. 2004; 552:219–246.
[20] DIAMOND Project Group. Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999. Diabet Med. 2006; 23:857–866.
[21] EURODIAB ACE Study Group. Variation and trends in incidence of childhood diabetes in Europe. Lancet. 2000; 355:873–876.
[22] Kamrath C, Tittel SR, Kapellen TM. Early versus delayed insulin pump therapy in children with newly diagnosed type 1 diabetes: results from the multicentre, prospective diabetes follow-up DPV registry. Lancet Child Adolesc Health. 2021; 5:17–25.
[23] Tandon N, Kalra S, Balhara YS. Forum for Injection Technique (FIT), India: The Indian recommendations 2.0, for best practice in insulin injection technique, 2015. Indian J Endocr Metab. 2015; 19:317–331.
[24] Jain SM, Pandey K, Lahoti A, Rao PK. Evaluation of skin and subcutaneous tissue thickness at insulin injection sites in Indian, insulin naı¨ve, type-2 diabetic adult population. Indian J Endocrinol Metab. 2013; 17:864–870.
[25] American Diabetes Association Professional Practice Committee. Diabetes care in the hospital: standards of care in diabetes-2024. Diabetes Care. 2024; 47:S295–S306.
[26] Vardar B, Kizilci S. Incidence of lipohypertrophy in diabetic patients and a study of influencing factors. Diabetes Res Clin Pract. 2007; 77:231e6.
[27] Lu Q, Li Y, Cai Z, Cui S, Shi Y. Homebased health management needs of children with type 1 diabetes mellitus in China: an information platform-based qualitative study. Transl Pediatr. 2020; 9:532–540.
[28] Owens J, Courter J, Schuler CL, Lawrence M, Hornung L, et al. home insulin pump use in hospitalized children with type 1 diabetes. JAMA Netw Open. 2024; 7:e2354595.
[29] Castaldini M, Saltmarch M, Luck S. The development and pilot testing of a multimedia CD-ROM for diabetes education. Diabetes Educ. 1998; 24:285–286.
[30] Cheng LH, Zhang YL, Zhong YJ. Effect of video guidance of insulin injection among diabetic patients. China Modern Doctor. 2016; 54:129–34.
[31] Celik S, Cosansu G, Erdogan S. Using mobile phone text messages to improve insulin injection technique and glycaemic control in patients with diabetes mellitus: a multi-center study in Turkey. J Clin Nurs. 2015; 24:1525–1533.
[32] Kamrul-Hasan A, Paul AK, Amin MN, Gaffar MAJ, Asaduzzaman M, et al. Insulin Injection Practice and Injection Complications - Results from the Bangladesh Insulin Injection Technique Survey. Eur Endocrinol. 2020; 16:41–48.
[33] Olamoyegun MA, Akinlade AT, Ala OA. Audit of insulin prescription patterns and associated burden among diabetics in a tertiary health institution in Nigeria. Afri Health Sci. 2018; 18:852–864.