Full Text
Introduction
During cesarean section, hypotension is a common physiological response with spinal anesthesia that have significant adverse maternal outcomes including nausea, vomiting, and dizziness with a 70% incidence rate [1]. Hypotension can be harmful to both the fetus as well as mother, like reductions in placental blood flow and fetal acidosis may occur as a result of prolonged hypotension. Timely management of low blood pressure with IV fluids or vasopressors is essential to prevent harmful effects on both mother and newborn.
Therefore, its common management recommends the use of vasopressors such as ephedrine, phenylephrine, and norepinephrine [2]. Study on these vasopressors provides a better response in lowering the incidence of fetal acidosis, vomiting, and nausea. On the other hand, phenylephrine considered a first-line agent assists in the reduction of cardiac output [3, 4].
Subjects and methods
This randomised double blinded study was conducted in a tertiary care teaching hospital after approval from the hospital ethics committee, and after obtaining written informed consent from patients between September 2022 and September 2023, for a duration of 13 months. One hundred and sixty term parturients between 20 and 30 years of age with singleton pregnancy belonging to the American Society of Anesthesiologists (ASA) physical class I and II posted for elective caesarean section under spinal anaesthesia were included in the study. Parturients with allergy or hypersensitivity to phenylephrine or norepinephrine, height <150 or >180 cm, any obstetric complications were excluded from the study.
On the day of surgery, 18-gauge intravenous cannula was inserted and standard monitoring with non-invasive arterial pressure, electrocardiography and pulse oximetry was established. The baseline vitals were noted. They were then loaded with 15 mL/kg of lactated Ringer’s solution. Subarachnoid block (at L3–L4 or L4–L5 level using standard technique) with 1.5 mL of 0.5% hyperbaric bupivacaine plus 0.5 mL of fentanyl was given using 23-G/ 25G, Quincke needle in the left lateral position or sitting. The patients were then put in supine with a wedge under the right buttock. Supplemental oxygen was administered via facemask at a flow rate of 4 liters per minute. The pinprick test was used to evaluate the maximum degree of sensory blockade attained.
The parturients were randomised into Group A and Group B by computer-generated randomised technique. Norepinephrine and phenylephrine were diluted and loaded in an identical coded 10-mL syringe to give norepinephrine 4 µg/mL and phenylephrine 50 µg/mL to treat post spinal hypotension and collected the data for analysis. The patient and the investigator were blinded to the vasopressor used. SBP, DBP, MAP, SPO2, HR were monitored every 2 min for the first 10 min, every 5 minutes for the next 30 minutes and every 10 minutes till the end of the surgery. Group A patients received phenylephrine 50µg as an intravenous bolus and Group B patients received 4µg of norepinephrine intravenous bolus whenever the systolic arterial pressure dropped below 20% of baseline. Following the birth of the baby, 10 units of oxytocin were administered through a slow infusion. Instances of lower blood pressure, lower or higher heart rate, hypertension, and the overall amount of vasopressor and intravenous fluid administered during the operation were recorded. Bradycardia was characterized by a heart rate below 50 beats per minute (bpm) and was managed with intravenous atropine at a dose of 0.6 mg. Tachycardia was characterized as a heart rate exceeding 120 beats per minute. Hypertension was characterized by a 20% rise in systolic blood pressure from the baseline, and its occurrence due to norepinephrine or phenylephrine boluses was recorded. A paediatrician unaware of the vasopressor employed recorded the Apgar score at 1 and 5 minutes. At birth, a sample from the umbilical vein was obtained for blood gas analysis, and the measurements of pH, PCO2, PO2, and lactates were evaluated.
Fetal acidosis was defined as pH <7. The time taken from skin incision to delivery of baby and the time taken from uterine incision to delivery of the baby and the total duration of surgery were noted. Incidences of dizziness, nausea or vomiting due to maternal hypotension were also noted.
The primary objective of our study was to compare the number of intravenous bolus doses of phenylephrine or noradrenaline required to treat spinal hypotension in caesarean patients. The secondary objectives were to compare the incidence of bradycardia, hypertension, nausea and vomiting in mother and foetal outcomes such as Apgar score and umbilical vein blood gases.
Results
The study included 180 patients who were randomly allocated into two equal groups by computer generated method. The study was conducted in the Department of Anaesthesiology, in a tertiary care centre, for a duration of 13 months. The patient demographic data was studied among the two groups and showed the following results.
The mean age of patients belonging to phenylephrine group (Group A) was 25.39±3.228 years, and noradrenaline group (Group B) was 24.94±2.892 years. The p value was 0.361, which suggests that the difference in age among the two groups was not statistically significant. The mean height for Group A and Group B was 154.43±2.894 cms and 156.73±2.3 cms, respectively and the p value of 0.324 suggests that the difference was not statistically significant. The mean weight for Group A and Group B was 63.78± 7.577 kgs and 63.19± 4.707 kgs, the p value of 0.526 was not statistically significant. The BMI for Group A was 23.804±3.74 and Group B was 22.74± 2.293, the p value for the difference was 0.2565, that was not statistically significant.
All patients achieved adequate spinal block height above T5, and the level of dermatomal height achieved was comparable between the groups. The duration of surgery required were also comparable between Group A and Group B. Intraoperative blood loss and total intravenous fluids transfused were comparable between the two groups (p value= 0.6854) (Table 1).
Table 1: Showing comparison of perioperative parameters among the two groups.
|
Parameters
|
Noradrenaline
|
Phenylephrine
|
P value
|
|
Onset of motor block in sec
|
13.13± 2.383
|
13.76±2.45
|
0.1012
|
|
Onset of sensory block in sec
|
8.4± 1.997
|
8.56±1.82
|
0.59
|
|
Duration of surgery in mins
|
65.25 ±12.924
|
65±10.36
|
0.8928
|
|
Total blood loss in mins
|
740±79.235
|
745± 80.975
|
0.6936
|
|
Total intravenous fluid in ml
|
1610± 133.692
|
1600.25±168.231
|
0.6854
|
|
Mean dose of vasopressor
|
2.13± 0.333
|
1.05± 0.219
|
0.001
|
Total dose of vasopressors (Figure 1) required to treat hypotension was lower in phenylephrine group (52.50±10.966 vs. 8.15 ± 1.571) and the difference was found to be statistically significant with p value 0.002. Changes in DBP (diastolic blood pressure) after administering vasopressors were presented in Figure 2. Incidence of bradycardia seen in Group A was comparable with Group B, but statistically not significant (Figure 3).
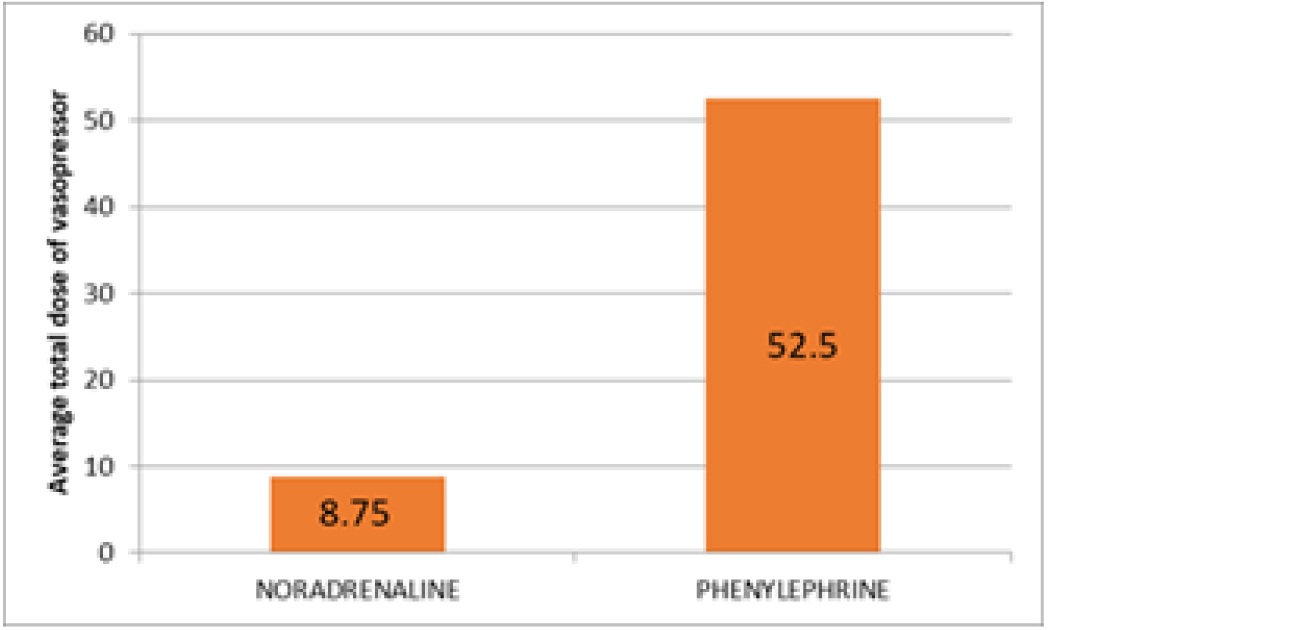
Figure 1: Total dose of vasopressor required to treat post spinal hypotension.
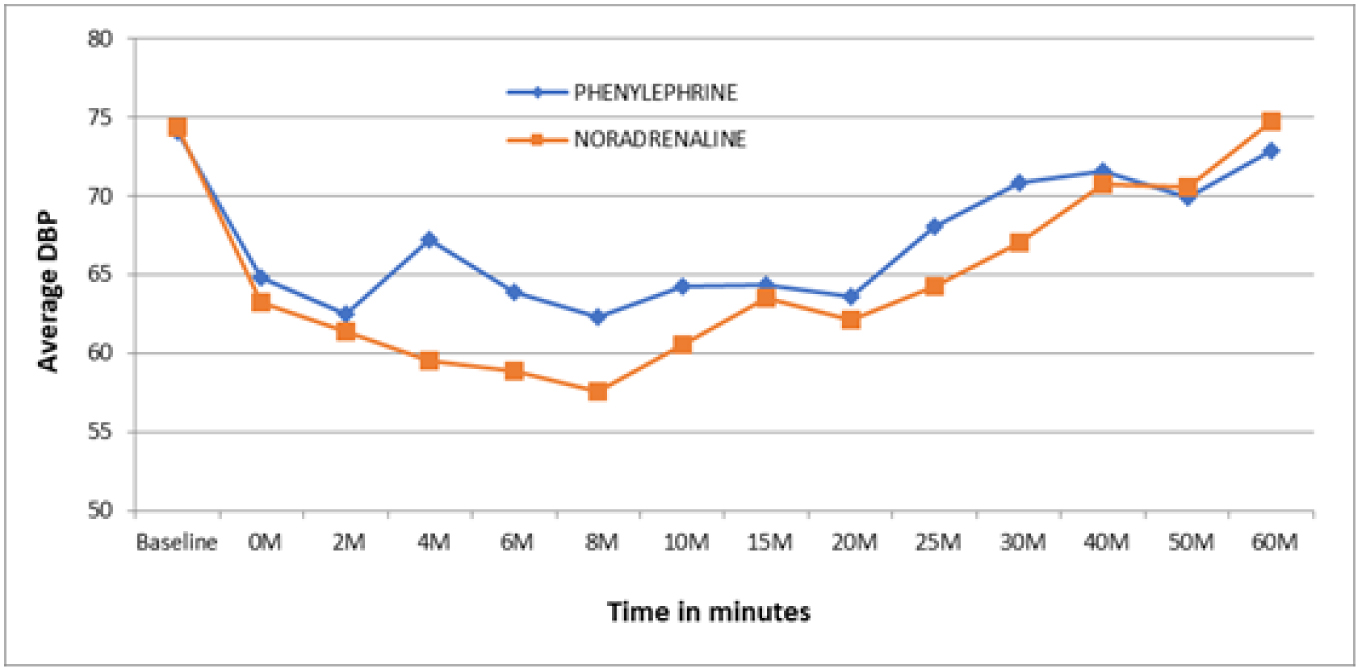
Figure 2: Changes in DBP (diastolic blood pressure) after administering vasopressors.
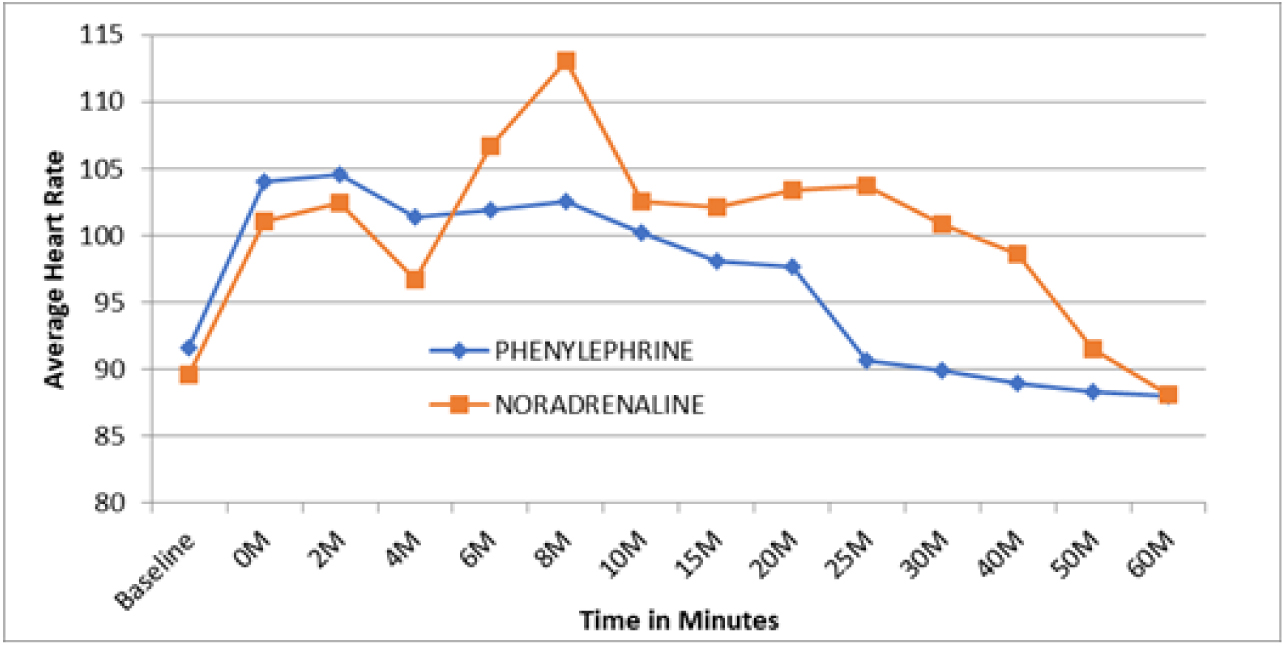
Figure 3: Changes in HR (heart rate) after administering vasopressors.
Maternal and foetal outcomes were compared with the two groups. Umbilical artery pH was 7.34± 0.41, and 7.338± 0.482, respectively for noradrenaline and phenylephrine groups and the p value was not statistically significant (p value= 0.9702). Similarly, the p value for PCo2, PO2 and lactates was 0.866, 0.683 and 0.683, respectively which were not statistically significant. The foetal parameters were compared using APGAR score at one minute and 5 minutes, p value was 0.189 and 0.4092, respectively and the difference was not statistically significant (Table 2).
Table 2: Showing comparison of parameters of maternal and fetal outcome among the two groups.
|
Parameters
|
Noradrenaline
|
Phenylephrine
|
P value
|
|
Umbilical artery pH
|
7.340 ± 0/041
|
7.338 ± 0.482
|
0.9702
|
|
pCO2
|
43.823 ± 5.864
|
43.711 ± 1.172
|
0.866
|
|
pO2
|
28.180 ± 9.421
|
27.672 ± 5.879
|
0.683
|
|
Lactates
|
1.929 ± 0.433
|
2 ± 1.494
|
0.6836
|
|
Apgar 1
|
8 ± 0.606
|
8.12 ± 0.640
|
0.189
|
|
Apgar 5
|
8.92 ± 0.277
|
8.88 ± 0.332
|
0.4092
|
The mean arterial pressure, systolic blood pressure and SPO2 after administering vasopressin were compared with the two groups and were not statistically significant (p value > 0.05 in each) (Figure 4, 5, and 6, respectively).
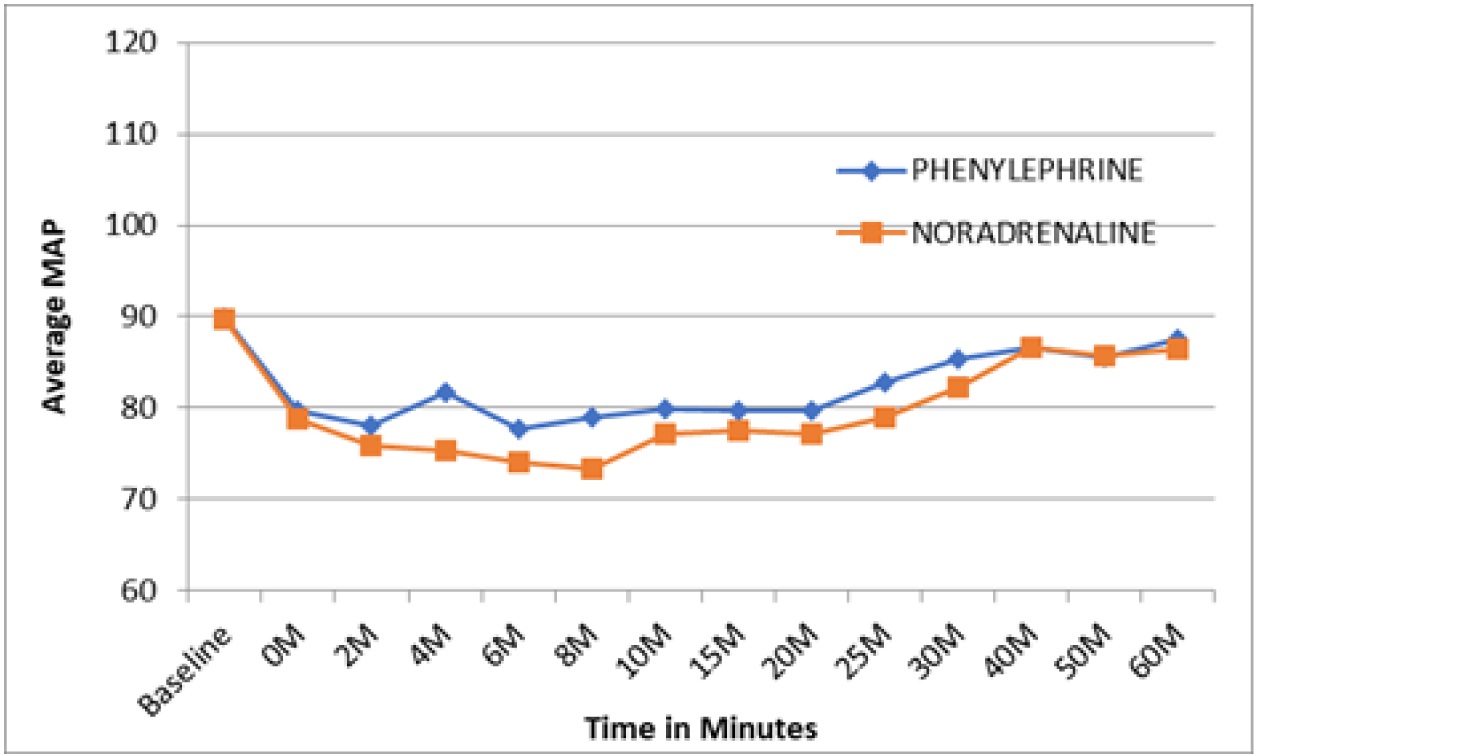
Figure 4: Changes in MAP (mean arterial pressure) after administering vasopressors.
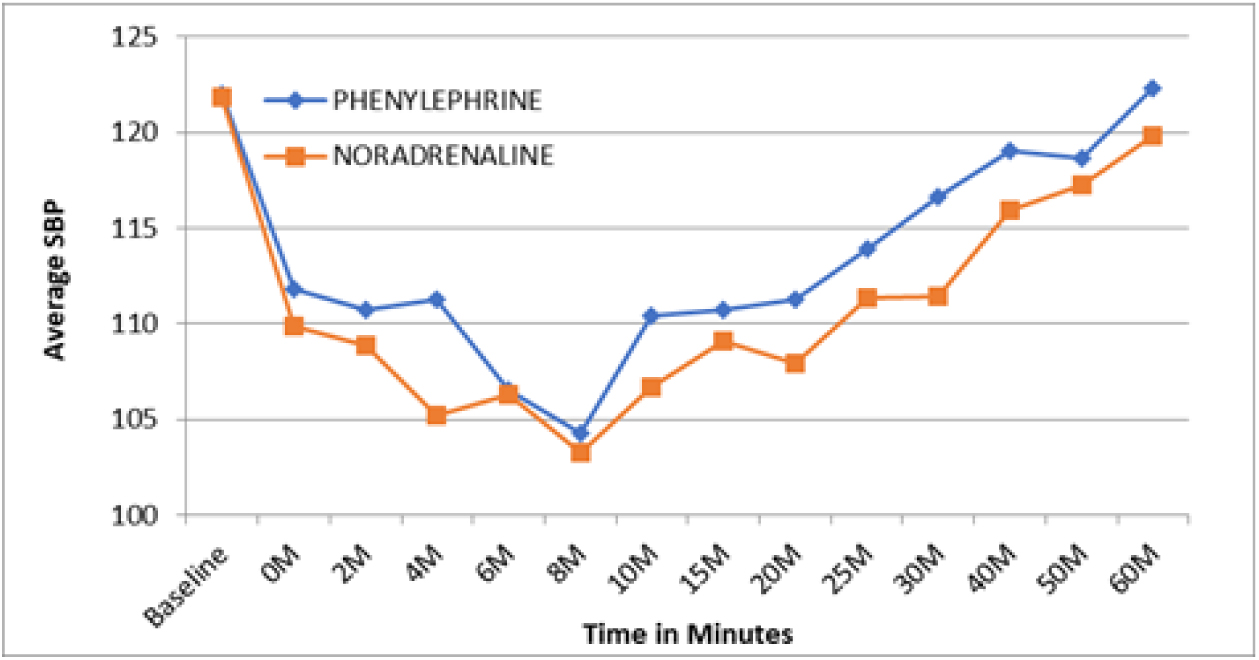
Figure 5: Changes in SBP (systolic blood pressure) after administering vasopressors.
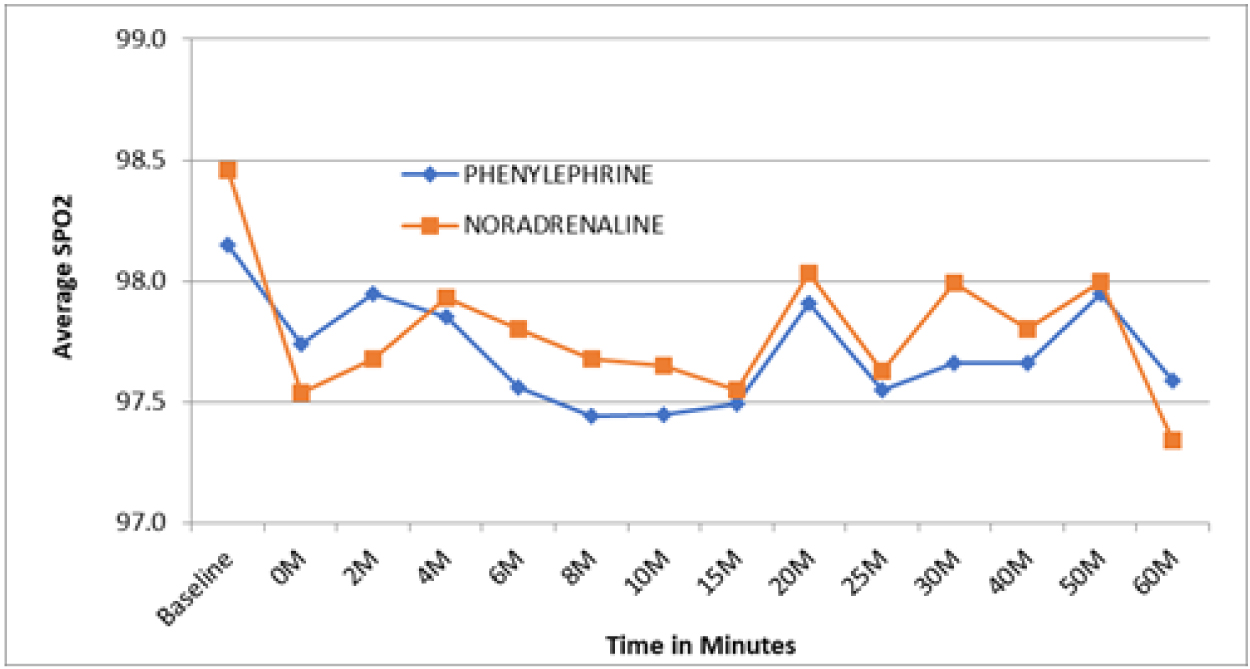
Figure 6: Changes in SPO2 (saturation) after administering vasopressors.
Discussion
Based on the results of the study by Kee et al., 4 µg of norepinehrine was found to be equipotent to 50 µg of phenylephrine [4]. Hence our Study compared the effects of intermittent bolus doses of phenylephrine (50mcg) and noradrenaline (4mcg) in the treatment of spinal hypotension during elective caesarean section.
According to Veeser et al., phenylephrine is the preferred drug for treatment of hypotension after spinal anesthesia for elective caesarean section, which agrees with the results of our study [5].
According to a randomised study done on total of one hundred twelve parturients by Sharkey et al., NE group had lower requirement of rescue bolus compared to PE group [NE-7.2% and PE- 21.4% ; P value < 0.03; difference (95% CI), -14.3% (-27.0% to -1.6%)] but similar maternal and fetal outcomes with NE compared to PE, including similar umbilical arterial and venous pH and blood gas values [6].
Mohtha, Gorg done a randomised study on 90 parturients and concluded that there was no difference in the incidence of bradycardia (37.8% with phenylephrine vs. 22.2% with noradrenaline; p = 0.167). Phenylephrine needed higher number of doses of drug (p value 0.01). The umbilical artery pH was higher using phenylephrine than with noradrenaline (p = 0.034). Hence both vasopressors reversed post spinal hypotension without a statistically significant difference in maternal bradycardia. However, in view of the lower umbilical artery pH when using noradrenaline, further research is warranted to study its placental transfer and fetal metabolic effects [7].
Even though there are certain literatures suggest norepinephrine is likely a promising alternative for rescuing maternal hypotension in obstetric anesthesia. Nonetheless, because of the limited number of studies currently available, it is premature to reach a conclusive decision. To ensure routine application in obstetric anesthesia, obtaining additional high-quality supporting data on NE is necessary [8].
Limitations of the study: This is a single institute study that was conducted on a small group of study population. Thus, we recommend the study trial to be conducted on a larger population to obtain the generalized data.
Conclusion
This study concludes that phenylephrine (50 μg) and norepinephrine (4 μg), when administered as intravenous bolus doses for treatment of post spinal hypotension in patients undergoing elective caesarean section, are associated with similar neonatal and maternal outcome and number of bolus doses required in treating hypotension are less with phenylephrine.
Acknowledgement
We thank the Department of Obstetrics and Gynaecology, MIMS, Mandya for their support in completion of study.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Mercier FJ, Augè M, Hoffmann C, Fischer C, Gouez AL. Maternal hypotension during spinal anesthesia for caesarean delivery. Minerva Anestesiol. 2013; 79:62–73.
[2] Chen D, Qi X, Huang X, Xu Y, Qiu F, et al. Efficacy and safety of different norepinephrine regimens for prevention of spinal hypotension in cesarean section: a randomized trial. Biomed Res Int. 2018; 2018:2708175.
[3] Kinsella SM, Carvalho B, Dyer RA, Fernando R, McDonnell N, et al. International consensus statement on the management of hypotension with vasopressors during caesarean section under spinal anaesthesia. Anaesthesia. 2018; 73:71–92.
[4] Kee WDN, Lee SW, Ng FF, Tan PE, Khaw KS. Randomized double–blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery. Anesthesiology. 2015; 122:736–745.
[5] Veeser M, Hofmann T, Roth LR, Klohr S, Rossaint R, et al. Vasopressors for the management of hypotension after spinal anesthesia for elective caesarean section. Systematic review and cumulative meta–analysis. Acta Anaesthesiol Scand. 2012; 56:810–816.
[6] Sharkey AM, Siddiqui N, Downey K, Xiang YY, Sharkey JG, et al. Comparison of intermittent intravenous boluses of phenylephrine and norepinephrine to prevent and treat spinal–induced hypotension in cesarean deliveries: Randomized controlled trial. Anesth Analg. 2019; 129:1312–1318.
[7] Mohta M, Garg A, Chilkoti GT, Malhotra RK. A randomised controlled trial of phenylephrine and noradrenaline boluses for treatment of postspinal hypotension during elective caesarean section. Anaesthesia. 2019; 74:850–855.
[8] Wang X, Shen X, Liu S, Yang J, Xu S. The Efficacy and safety of norepinephrine and its feasibility as a replacement for phenylephrine to manage maternal hypotension during elective cesarean delivery under spinal anesthesia. Biomed Res Int. 2018; 2018:1869189.