Orginal Research
2024
June
Volume : 12
Issue : 2
Retrospective analysis of laparoscopic and open orchidopexy for non palpable intra-abdominal testes in a tertiary care centre
Thoker MA, Mushtaq M, Thoker AH, Ahmed M, Malik SA
Pdf Page Numbers :- 143-147
Mukhtar Ahmad Thoker1, Mosin Mushtaq1,*, Ashaq Hussain Thoker2, Manzoor Ahmed1 and Sajad Ahmad Malik3
1Department of Minimal Access and General Surgery, Government Medical College, Shri Maharaja Hari Singh Hospital, Srinagar, Jammu and Kashmir 190010, India
2Department of Paediatrics, Director Health Services, Jammu and Kashmir 180001, India
3Department of Urology, Sheri Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir 190011, India
*Corresponding author: Dr. Mosin Mushtaq, Assistant Professor, Department of Minimal Access and General Surgery, Government Medical College, Shri Maharaja Hari Singh Hospital, Srinagar, Jammu and Kashmir 190010, India. Email: mozn33@gmail.com.
Received 27 January 2024; Revised 15 March 2024; Accepted 21 March 2024; Published 27 March 2024
Citation: Thoker MA, Mushtaq M, Thoker AH, Ahmed M, Malik SA. Retrospective analysis of laparoscopic and open orchidopexy for non palpable intra-abdominal testes in a tertiary care centre. J Med Sci Res. 2024; 12(2):143-147. DOI: http://dx.doi.org/10.17727/JMSR.2024/12-27
Copyright: © 2024 Thoker MA et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: Patients with non-palpable testes has numerous treatment options, the most effective treatment is still controversial. Laparoscopy has nowadays gained the trust as the most reliable modality for the management of impalpable testis. The aim of our study was to retrospectively analyse the laparoscopic and open orchidopexy procedures and report the outcome of our series.
Material and methods: 120 patients with 130 non palpable testes with a mean age of patients about 2.7 years who had undergone orchidopexy by open and laparoscopic methods over past 8 years.
Results: Mean age of open group was similar to laparoscopic group (2.7 ± 1.7 vs 2.5 ± 1.5 years; p > 0.05). 10 patients (8.33%) presented with bilateral non palpable testes. 10 testes from the open group and 8 from the laparoscopic group were of vanishing variety. Fowler -Stephens staged procedure was done for 4 testes in laparoscopic group. The mean operative time was more in the laparoscopic group than the open (63min vs 47min). Laparoscopic orchidopexy group had generally lesser use of analgesics. The mean hospital stay between the open and laparoscopic groups was 2.1 vs 1.3 days (p <0.05). 12 cases of testicular atrophy were noted, 7 from the open group and 5 from the laparoscopic group.
Conclusion: Results of open and laparoscopic orchidopexy procedures were fairly constant. Although, laparoscopy gives significantly less morbidity, is less painful, has lesser hospital stay and is cosmetically better.
Keywords: cryptorchidism; laparoscopy; orchidopexy; testis
Full Text
Introduction
Cryptorchidism meaning hidden testes, is one of the most common congenital anomalies, occurring in 1% to 4% of full-term and 1% to 45% of preterm male neonates. It can occur in isolation or as a part of a syndrome [1, 2]. Undescended testis is divided into palpable and non palpable groups. Testes that are ectopic, retractile, high scrotal, confined to the inguinal canal and located in the deep inguinal ring are mostly palpable. The non-palpable testis may present as agenesis, vanishing testes, intra-abdominal testes or inguinal testes [3, 4]. The etiology of cryptorchidism is multifactorial. Some of the involved factors are weight at birth to age one year independent of the length of gestation [5], familial history of cryptorchidism, variable growth of vertebrae and pelvis until 23 weeks of gestation, development of the gubernaculum, processus vaginalis, spermatic vessels and scrotum, decreased intraabdominal pressure during gestation leading to failure in descent of testis. A normal levels of sex hormones like testosterone is also a prerequisite for testicular descent [6-8]. Right undescended testis is more common about 50% while left undescended testis is seen in 25% and bilateral also seen in 25% of cases [9]. Physical examination of the testis can be difficult at times and imaging modalities like ultrasonography, computed tomography and magnetic resonance imaging may be needed if a testis cannot be definitely identified.
Correction of cryptorchidism is indicated to optimize testicular function, potentially reduce and/or facilitate diagnosis of testicular malignancy, provide cosmetic benefits and prevent complications such as clinical hernia or torsion. The present recommended age for surgical correction of undescended testis is 6 months in full term males. The standard treatment for undescended testes is orchidopexy using open or laparoscopic repair. In experienced hands, laparoscopy has nowadays become standard procedure in the management of non palpable intra-abdominal testis.
The aim of our study is to compare the outcome of laparoscopic and open orchidopexy for impalpable intra-abdominal testis managed at our center over a period of eight years.
Material and methods
The present study is a retrospective analysis of patients with impalpable intra-abdominal testis managed between January 2016 and December 2023 at Sheri Kashmir Institute of Medical Sciences, Srinagar, Jammu & Kashmir, India. Analysis of records of 120 patients was done in this study. Out of these 60 patients were managed by open orchidopexy and another 60 patients were managed by laparoscopic orchidopexy. Medical records of all these patients were studied and recorded in a pre-designed proforma and the data was subsequently analysed. The patients were in the age group of 7 months to 11 years, mean age of open group was similar to laparoscopic group (2.7 ± 1.7 vs 2.5 ± 1.5 years). Majority of the patients were diagnosed on the basis of history, local examination of the genital area along with abdominal and scrotal ultrasonography confirming clinical examination. Magnetic Resonance Imaging (MRI) was used in some patients for diagnosis and exact localization of testis in the abdomen as MRI is considered as imaging modality of choice for non palpable intra abdominal testis. MRI does not involve ionizing radiation, making it safer for pediatric patients. MRI and then subsequent laparoscopic findings in our study were correlating with each other especially regarding location of testis. In our study, we included all children up to the age of 11 years with unilateral or bilateral non palpable testes and excluded all children having palpable undescended testis. This study was approved by the ethical committee of our institute.
Technique
Laparoscopic orchidopexy: Inguinal examination was performed in each child under anaesthesia to confirm the preoperative diagnosis. The primary 10mm camera port is introduced by closed technique at superior margin of umbilicus and pneumoperitoneum established (10mmHg), the area of the internal inguinal ring is inspected bilaterally and subsequent trocars (two 5mm) placed under laparoscopic visualization. After visualizing all the abdominal quadrants, if intra-abdominal blind ending cord structures were found, no further exploration was performed and a diagnosis of intra-abdominal vanishing testes was made. If an intra-abdominal testis was found, it was classified as high and low depending on its position to the internal ring (Figure 1). For intra-abdominal testis gubernacular attachment is divided as shown in Figure 2. Once the testis had been adequately mobilized which was confirmed by performing stretch manoeuvre (which is a technique used to increase the mobility of an undescended testis, facilitating its placement into the scrotum. It includes dissection and mobilization of spermatic vessels and vas deferens, stretching and pulling of testis and spermatic cord and assessment of tension on spermatic vessels which could compromise blood flow or cause testicular damage) the dissection was further carried out medially all around the ring to complete the herniotomy. The pathway to the ipsilateral hemiscrotum was created by passing a blunt tip of the laparoscopic dissector over the pubic bone into the ipsilateral hemiscrotum (Figure 3). A dartos pouch was prepared in the hemiscrotum. The testis was grasped ensuring that only gubernacular tissue was grasped. The testes was brought out into the scrotum and the length checked by deflating the abdomen. Testes was fixed in scrotum using 5-0 chromic catgut suture. At the end of the procedure, abdomen was examined for any bleeding, the pneumoperitoneum released, trocars removed. Trocar sites were closed.
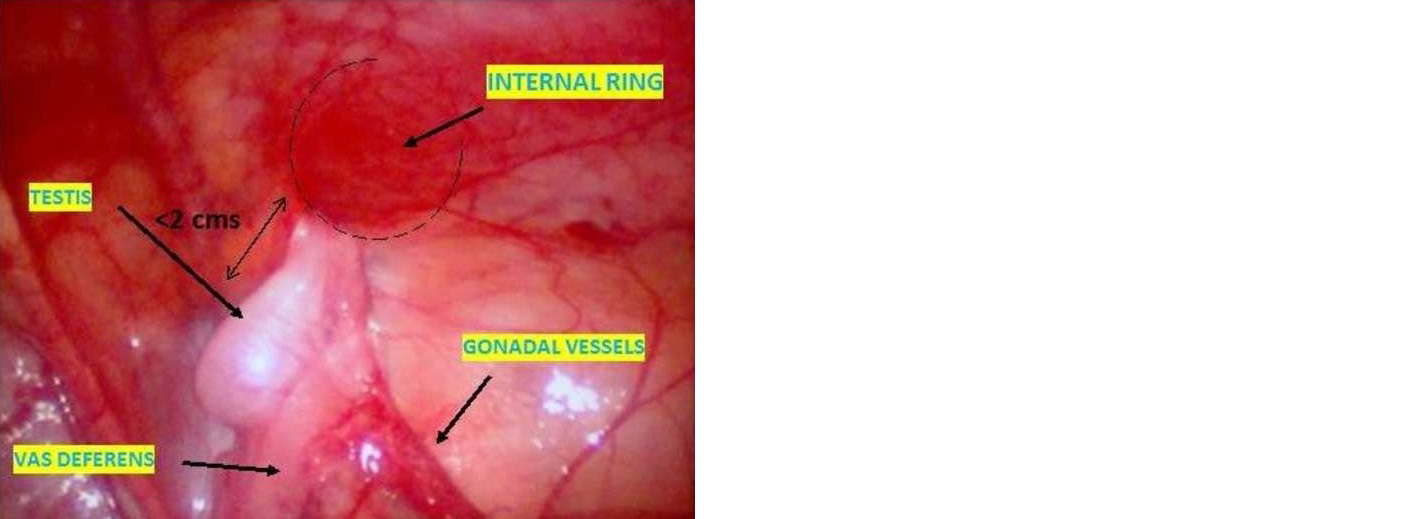
Figure 1: Intra-abdominal testis less than 2 cms from the deep ring.
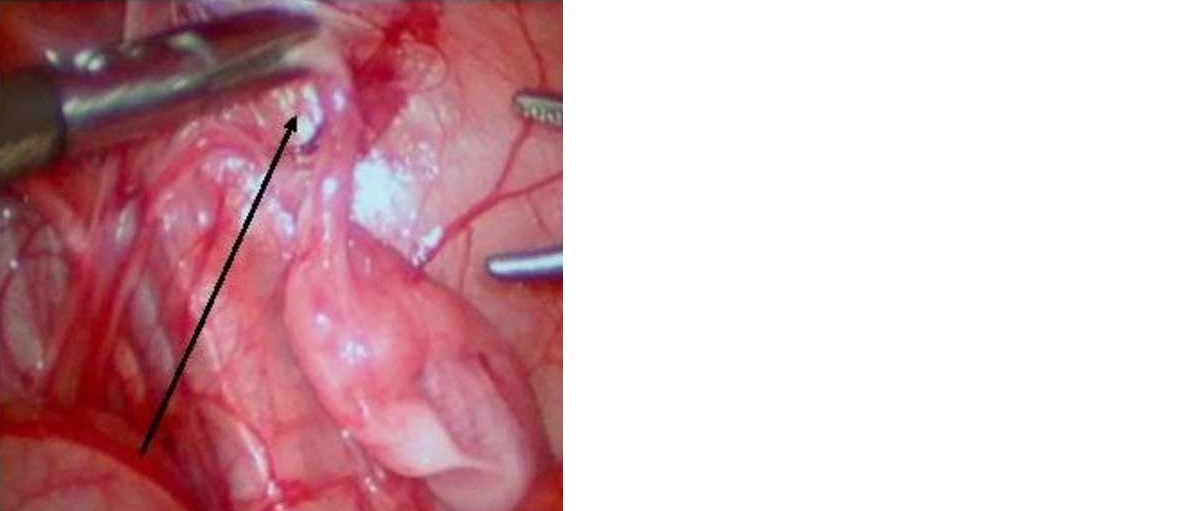
Figure 2: Gubernaculum forming a handle for mobilizing the testis.
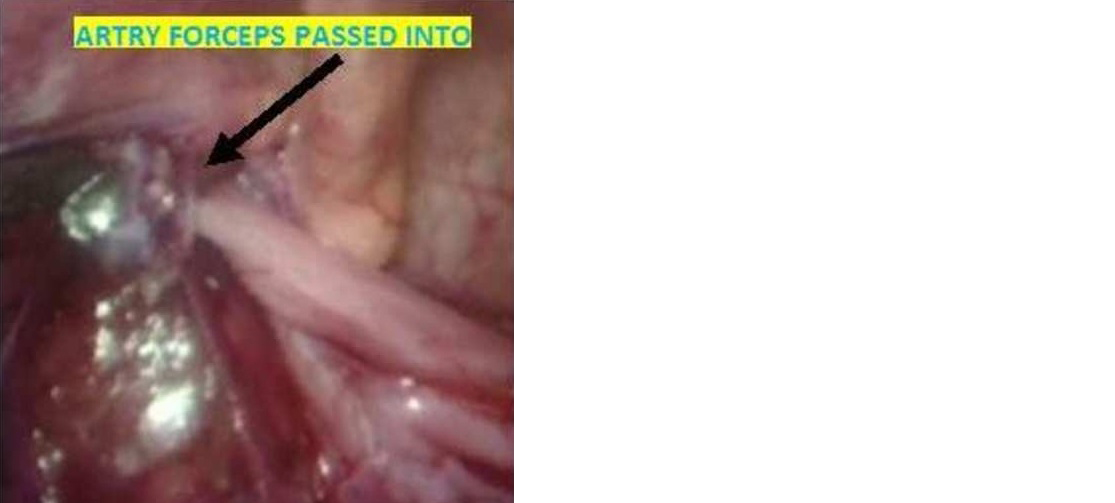
Figure 3: Pull through of the mobilized testis.
Open orchidopexy: Preoperative preparation and anesthesia protocols for open orchidopexy mirrored those employed in laparoscopic orchidopexy. The patient was positioned in supine and under all aseptic precautions an inguinal crease incision was made into the abdomen and another was made in the scrotum. Through the deep ring a retroperitoneal and intraperitoneal exploration was carried out and the testis was detached from surrounding tissues and pulled out of the abdominal incision attached to the spermatic cord. The testis is then pulled down into the scrotum, and stitched into place (Figure 4).

Figure 4: Scrotal placement of testis in open orchidopexy.
Statistical analysis
Data was entered into Microsoft Excel spreadsheet. The said data was coded and exported to data editor of Statistical Package for Social Sciences (SPSS Ver. 23).Categorical variables were described as frequencies and percentages while as continuous variables as mean with standard deviation. The statistical significance of the variance between two independent groups in continuous variables was assessed using an unpaired Student’s t-test. To examine the notable disparity in proportions between two groups for qualitative data, the Chi-square test was utilized. A significance threshold of p < 0.05 was deemed as noteworthy.
Results
120 patients with 130 non palpable undescended testes were enrolled in the study. Ten patients presented with bilateral non palpable undescended testes. Patients were randomly divided into two equal groups of open orchidopexy and laparoscopic orchidopexy. Mean age of open group was similar to laparoscopic group (2.7 ± 1.7 vs 2.5 ± 1.5 years; p value 0.495). Comparison of preoperative and intraoperative findings between two groups are summarized in Table 1.
Table 1: Comparison of Preoperative and Intraoperative findings in both groups.
|
Parameter
|
Open Group
|
Laparoscopy Group
|
|
No. of patients
|
60
|
60
|
|
No. of non palpable testis
|
66
|
64
|
|
Side of involvement
|
| |
Right side
|
32 (53.33%)
|
36 (60%)
|
| |
Left side
|
22 (36.66%)
|
20 (33.33%)
|
| |
Bilateral
|
6 (10%)
|
4 (6.66%)
|
|
Intra operative location of testis
|
| |
Peeping testis
|
32
|
30
|
| |
Low abdominal
|
16
|
18
|
| |
High abdominal
|
2
|
4
|
| |
Vanishing testis
|
10
|
8
|
|
Intra operative complications
|
| |
Port side bleed
|
NA
|
2
|
| |
Testicular artery injury
|
0
|
2
|
| |
Pampiniform plexus injury
|
5
|
0
|
| |
Mean operative time (minutes)
|
47
|
63
|
Ten testes from the open group and 8 from the laparoscopic group were of vanishing variety. Fowler –Stephens staged procedure was done for 4 testes in laparoscopic group. The mean operative time was more in the laparoscopic group than the open cohort (63min vs 47min) and the difference was statistically significant (p value 0.001). There were no major intra-operative complications in the either group. Minor complications included port site bleed in two patients from the laparoscopic cohort which was managed conservatively by using laparoscopic monopolar diathermy, two patients from the same cohort had injury to the testicular artery which were then clipped using LT 300 titanium clips. All the laparoscopic procedures were completed successfully without the need for conversion. There were five complications in the open cohort in the form of bleeding from pampiniform plexus which were managed with monopolar electrocautery. There was no significant difference in the timing of return of bowel function and resumption of oral intake between the open and the laparoscopic group. The post operative details between two groups are tabulated in Table 2.
Table 2: Post operative details between two groups.
|
Parameter
|
Open Group n = 60
|
Laparoscopic Group, n = 60
|
p value
|
|
Superficial wound infection
|
4
|
2
|
0.402
|
|
Subcutaneous emphysema
|
0
|
2
|
0.15
|
|
Hydrocele
|
2
|
4
|
0.4
|
|
Testicular atrophy
|
7
|
5
|
0.54
|
|
Pain relief (Mean no. of
analgesic doses)
|
2.3
|
1.2
|
0.001
|
|
Mean hospital stay (in days)
|
2.1
|
1.3
|
0.001
|
|
Mean follow up (in Months)
|
8.3
|
7.5
|
0.0001
|
|
Mean return to activity (in weeks)
|
1.5
|
1.1
|
0.32
|
In the open group, early postoperative complications such as superficial wound infection and hydrocele were notably more severe, contributing significantly to prolonged hospital stays and increased morbidity. The complications were statistically insignificant between these two groups with a p value for all early postoperative complications >0.005. In the laparoscopic orchidopexy group, there was generally less reliance on analgesics (p value of 0.001), with the majority of patients being discharged within the first postoperative day (p value of 0.001). During long-term follow-up, 12 patients experienced testicular atrophy, with 7 from the open group and 5 from the laparoscopic group. All patients from both groups were rigorously monitored post-surgery at consistent intervals: weekly for the first month, at 6 weeks, and at 6 months. Overall, parents of patients who underwent laparoscopic surgery reported higher satisfaction levels. There was no significant difference in return of normal active life between two groups with p value of 0.32. The laparoscopic procedure incurred significant expenses primarily due to the utilization of disposable trocars. Nonetheless, the shorter hospitalization, decreased morbidity, and quicker recovery period are anticipated to result in reduced overall costs.
Discussion
Cryptorchidism is one of the commonest abnormality of male sexual development. In this condition, the testis is absent from scrotum. Cryptorchidism may have a deleterious effect upon testicular development when left untreated. If treated early, the effect of core body temperature will be shorter and the testes grow much better than those not operated on during the first 24 months of life, limiting the risk of azoospermia [3], as well as allowing easy access for self examination and mitigating esthetic and psychological problems [1]. Presently, nearly all specialists advocate for early intervention to address cryptorchidism. Despite the availability of numerous treatment strategies for boys with non-palpable testes, there persists a debate regarding the most efficacious approach. Traditionally, an open inguinal exploration would have been undertaken to locate the missing testis, followed by a conventional orchidopexy or orchidectomy [10, 11]. Laparoscopy is recognized as the most dependable diagnostic method for handling impalpable testes. It offers a clear visualization of anatomy and furnishes visual data crucial for making definitive decisions. [12]. Diagnostic laparoscopy and laparoscopic orchidopexy has begun to surpass surgical exploration as the primary treatment in boys with impalpable testes, gaining wide acceptance in the urologic and pediatric surgery circles, it is widely acknowledged that surgery is the most efficient approach for relocating an intra-abdominal testis to a dependent position [13-15].
Typically, the higher the testis is positioned, the more challenging its repositioning becomes, leading to a lower success rate [2]. This is because surgeons must conduct a broader dissection to liberate the testis and its cord and to achieve a longer stalk. However, retroperitoneal extension of the dissection often provides adequate mobilization, enabling scrotal placement in the majority of cases. A number of studies have compared open orchidopexy with laparoscopic orchidopexy for non palpable testes and results found are consistently similar with our experience in relation to age group selected [16-19], side determination of undescended testis [18-21], preoperative investigation protocol for localisation of testes [5, 20-22], the mean operative time [1, 7, 14], the time of starting the oral feeds after surgery [1], post surgical complications observed in either group [1, 9, 15], the average postoperative hospital stay [2] and time taken to return to daily activities.
Limitations of our study: This study was conducted in a tertiary care center with a limited patient population. Multi-center studies involving a larger number of patients are necessary for more precise results. Data from a tertiary care center may not accurately reflect the disease profile of the broader community. Acknowledging this limitation, the current study's findings are based on a small sample size and are insufficient to draw definitive conclusions.
Conclusion
Laparoscopy is diagnostic modality of choice for localisation of non-palpable intra-abdominal testis. Laparoscopy is good for high undescended testis, as mobilization of cord can be done without any extensive dissection in contrast to open orchidopexy technique. Results of open and laparoscopic orchidopexy procedures are fairly constant. However, laparoscopy results in significantly lower morbidity, causes less pain, requires a shorter hospital stay, and offers better cosmetic outcomes.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Chui CH, Jacobson AS. Laparoscopy in the evaluation of the non-palpable undescended testes. Singapore Med J. 2008; 41:206–208.
[2] Koyama T, Nonomura K, Ameda K, Kakizaki H, Yaksuni. Laparoscopic Evaluation & Management of the Nonpalpable Testis. Diagn Ther Endosc. 1997; 4:69–74.
[3] Corvin S, Sturm W, Anastasiadisa A, Kuczyk M, Stenzl A. Laparoscopic management of adult non-palpable testicle. Urol Int. 2005; 75:337–339.
[4] Hinyokika N, Zasshi Z. Management of impalpable testis: The value of laparoscopy for subsequent treatment. BJU 1991; 82:125–132.
[5] El-Gohary MA. The role of laparoscopy in the management of impalpable testes. Pediatric Surg Int. 1997; 13:463–465.
[6] Hali WO. Management of impalpable testis. Indications for abdominal exploration. J Pediatric Surg. 1997; 32:918–920.
[7] Mark SD. The role of laparoscopy in evaluation of the impalpable undescended testes. Aust NZJ Surg. 1997; 67:332–334.
[8] Hay SA. Laparoscopic classification and treatment of the impalpable testis. Paediatric Surg Int. 1999; 15:570–572.
[9] Lindgren BW, Franco I, Bilick S, Selwyn B, William A, et al. Laparoscopic Fowler Stephens Orchidopexy for the high abdominal testis. J Urol. 1999; 162:990–994.
[10] Masao T, Osamu M, Kazuhiro Y, Kenichi K, Kiyomi M. Laparoscopy in diagnosis and treatment of non-palpable testis. Int J Urol. 2001; 8 692–696.
[11] Van Savage JG. Avoidance of inguinal incision in laparoscopically confirmed vanishing testis syndrome. J Urol. 2001; 166:1421–1424.
[12] Baniegbhal B. Laparocopic Orchidopexy. JPGM. 2005; 51:268. [13] Schlett H. Groin exploration for non-palpable testis: Laparoscopic approach. J Pediatric Surg. 2002; 37:1552–1556.
[14] Argos RMD, Unda FA, Orpez RA, Lorenzo GC. Diagnostic and therapeutic laparoscopy for nonpalpable testis. Surgical Endoscop. 2003; 17:1756–1758.
[15] Mehta KD, Kacheriwala SM, Jain RY, Pillai B, Sodhi AP. Management of impalapable testis: Laparoscopic approach. Indian J Surgery. 2003; 65:430–434.
[16] Satar N, Bayazit Y, Doran S. Laproscopy in management of impalpable testicle. Acta Chir Belg. 2005; 105:662–666.
[17] Hvistendahl GM, Poulsen EU. Laparoscopy for impalapable testis: Experience with 80 intra abdominal testis. J Pediatr Urol. 2009; 5: 389–392.
[18] Ismail K, Ashour M, El-Afifi M, Hashish A. Laparoscopy in the management of impalpable testis. World J Surg. 2009; 33:1514–1519.
[19] Hassan ME, Mustafawi A. Laproscopic management of impalpable testes in children –new classification; lessons learned and rare anomalies. Lapro endosc Adv Surg. 2010; 20:265–269.
[20] Guo J, Liang Z, Zhang H, Yang C, Pu J, et al. Laparoscopic versus open orchiopexy for non-palpable undescended testes in children: a systemic review and meta-analysis. Pediatric Surg Int. 2011; 27:943–952.
[21] Wayne C, Chan E, Nasr A. What is the ideal surgical approach for intra-abdominal testes? a systematic review. Pediatr Surg Int. 2015; 31:327–338.
[22] Salah E, Elssayed A. The role of laparoscopy in non-palpable undescended testicle: analysis and review of the experience from two cities in Sudan. Afr J Paediatr Surg. 2022; 19:127–132.