Full Text
Introduction
Anaesthesia for caesarean section can be administered either as general or regional anaesthesia, each having its own advantages and disadvantages. General anaesthesia is associated with risks such as aspiration pneumonia, failed intubation, and respiratory complications in both mother and newborn [1]. Spinal anaesthesia offers advantages such as rapid onset, effective postoperative analgesia, lower cost, and safety, with patients remaining awake and having a lower risk of aspiration. It involves the administration of local anaesthetic into the subarachnoid (intrathecal) space. This technique has a high success rate, quick onset, and consistent block, particularly with hyperbaric solutions. However, spinal anaesthesia is associated with hypotension due to sympathetic blockade [2]. Hypotension is defined either as a systolic blood pressure <90 mmHg or a decrease of more than 20% from baseline. It is commonly managed using intravenous fluids and vasopressors [3]. Oxytocin is routinely administered after placental delivery to enhance uterine contractility and reduce postpartum haemorrhage [4]. However, bolus administration of oxytocin may cause significant hypotension, due either to reduced cardiac output from decreased venous return or reduced systemic vascular resistance [5].
Phenylephrine is a selective alpha-1 adrenergic receptor agonist and is effective in increasing mean arterial pressure. It is commonly administered as a 50-100 mcg IV bolus, with a rapid onset (1-3 minutes) and short duration (5-20 minutes) [6, 7]. Mephentermine is a mixed-action sympathomimetic agent, acting both directly and indirectly on alpha and beta receptors. Its predominant beta-agonist action increases blood pressure mainly by enhancing cardiac output. It is commonly administered in 3-5 mg IV boluses or as a 2-5 mg/min infusion [8].
There is limited literature evaluating the effective dose of phenylephrine and mephentermine for preventing oxytocin-induced hemodynamic changes. Therefore, this study aims to compare the efficacy of phenylephrine and mephentermine in preventing such changes during LSCS under spinal anaesthesia.
Materials and methods
This randomized controlled study was conducted in the department of Anaesthesiology at Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh for the duration of one year from August 2023 to July 2024, after approval from the Institutional ethics committee. In the study, a total of 64 female patients aged between 18-40 years and classified as ASA physical status II were taken as study participants, who were scheduled for elective LSCS under spinal anaesthesia. The sample size was calculated using the software power & sample size program using results obtained in a study by Kumar et al [13] on similar groups with Alpha- 5%, Power- 70%, P0- 22%, P1- 5%. Where P0 is proportion of outcome in group 1 and P1 is proportion of outcome in group 2. The sample size came out to be 32 patients in each group. Patients with a known allergy to local anaesthetics, a baseline heart rate of less than 60 beats per minute, baseline blood pressure below 100/60 mmHg, any history of bleeding diathesis or coagulopathy, and the presence of septic shock, were excluded from the study.
Written informed consent was obtained from all the patients as well as a thorough pre-anaesthetic check-up was conducted a day prior to the surgery. Study participants were randomly allocated to two groups, A & B. Patients were randomly divided in two groups in 1:1 allocation ratio a day prior to surgery, and the drugs were prepared by the anaesthetist who wasn’t involved in the observation. Patients were administered tablet ranitidine 150 mg the night before surgery and were kept nil per oral (NPO) 8 hours for solids and 2 hours for clear liquids. Preoperatively, 18 gauze IV cannula was secured and crystalloid fluid was started at the rate of 10 ml/kg over 30 minutes. Maintenance fluid was administered as per the Holliday-Segar formula. Baseline vitals including heart rate, SBP, DBP, MAP, SpO2, and ECG were recorded. A dose of 10 mg of 0.5% hyperbaric bupivacaine was administered as spinal anaesthesia under aseptic precautions at the L2-L3 or L3-L4 intervertebral space using a 25 G Quincke needle. Following spinal anaesthesia, patient was positioned supine, and oxygen was delivered via face mask at the rate of 6 L/min. Any episode of hypotension following spinal anesthesia was managed as per the institutional protocol by either a fluid bolus of 100ml or by mephentermine 6mg IV.
Just before cord clamping, group A patients were given an IV bolus of 75 mcg phenylephrine while group B patients received an IV bolus of 6 mg mephentermine. After cord clamping, oxytocin 3 IU IV bolus over 1 minute was administered to all the patients. Hemodynamic parameters were observed and recorded every minute for 5 minutes. Details of patients such as ASA grade, diagnosis, procedure performed, and other relevant medical history were collected. Hemodynamic changes (heart rate, SBP, DBP, MAP) were noted. All off the information and observations were entered in Microsoft Excel spreadsheet and interpreted with SPSS software version 23.0.
Results
A total of 64 patients were included in this study which were randomly allocated into two groups, 32 patients in each group. The mean ages were 26.6 years (SD = 4.18) for the mephentermine group and 27.8 years (SD = 4.84) for the phenylephrine group. The chi-square test showed no statistically significant difference in the age distribution between the two groups (χ²=3.19, p=0.363), indicating that the age did not influence the choice of drug administered (Figure 1).
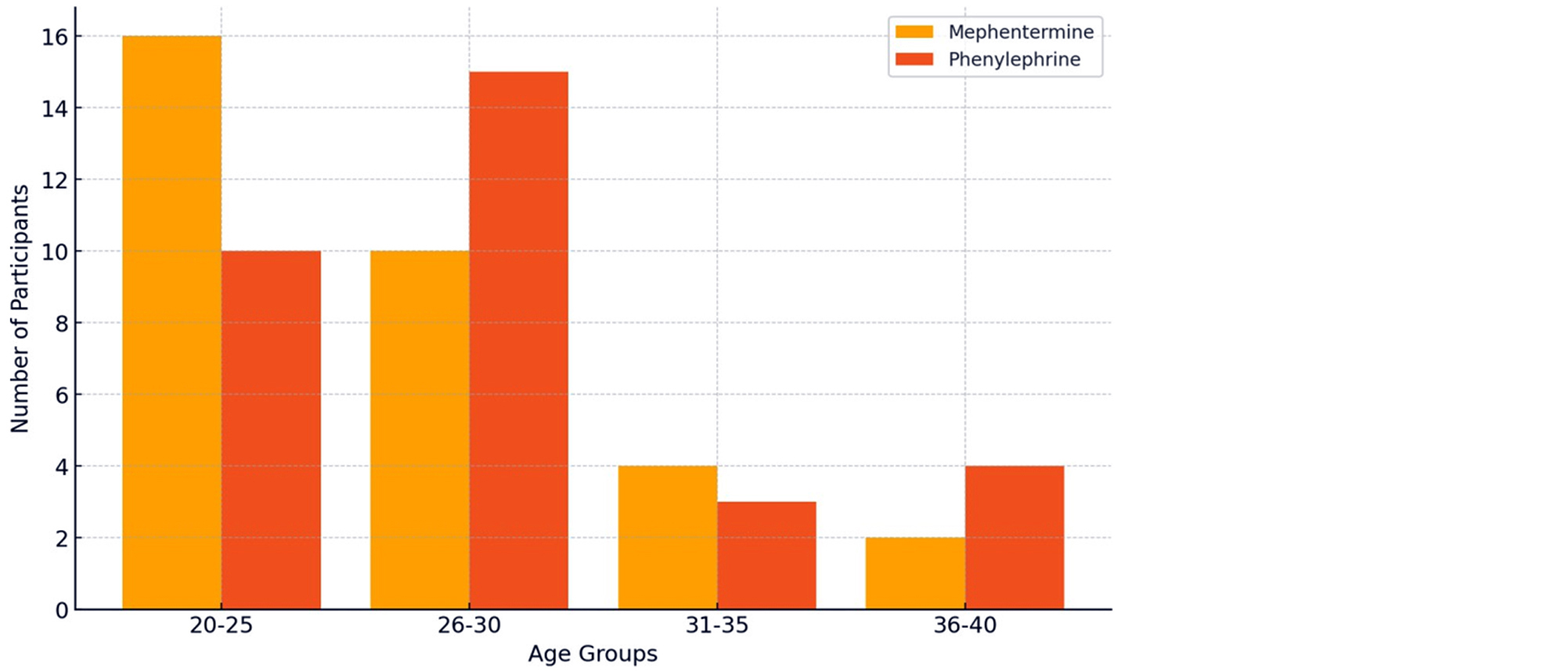
Figure 1: Distribution of study participants according to age.
The mean weight was obtained for both the groups and it was observed that the mean weight for the Mephentermine group was 57.3 kg (95% CI: 53.7–60.9 kg, SD±10.05 kg), while the Phenylephrine group had a mean weight of 56.4 kg (95% CI: 53.4–59.5 kg, SD ± 8.51 kg). It was evaluated that the weight of patients was not statistically significant (t-value of 0.362 and p-value of 0.718) and observed variation in mean weights was likely due to random chance rather than a true difference (Figure 2).
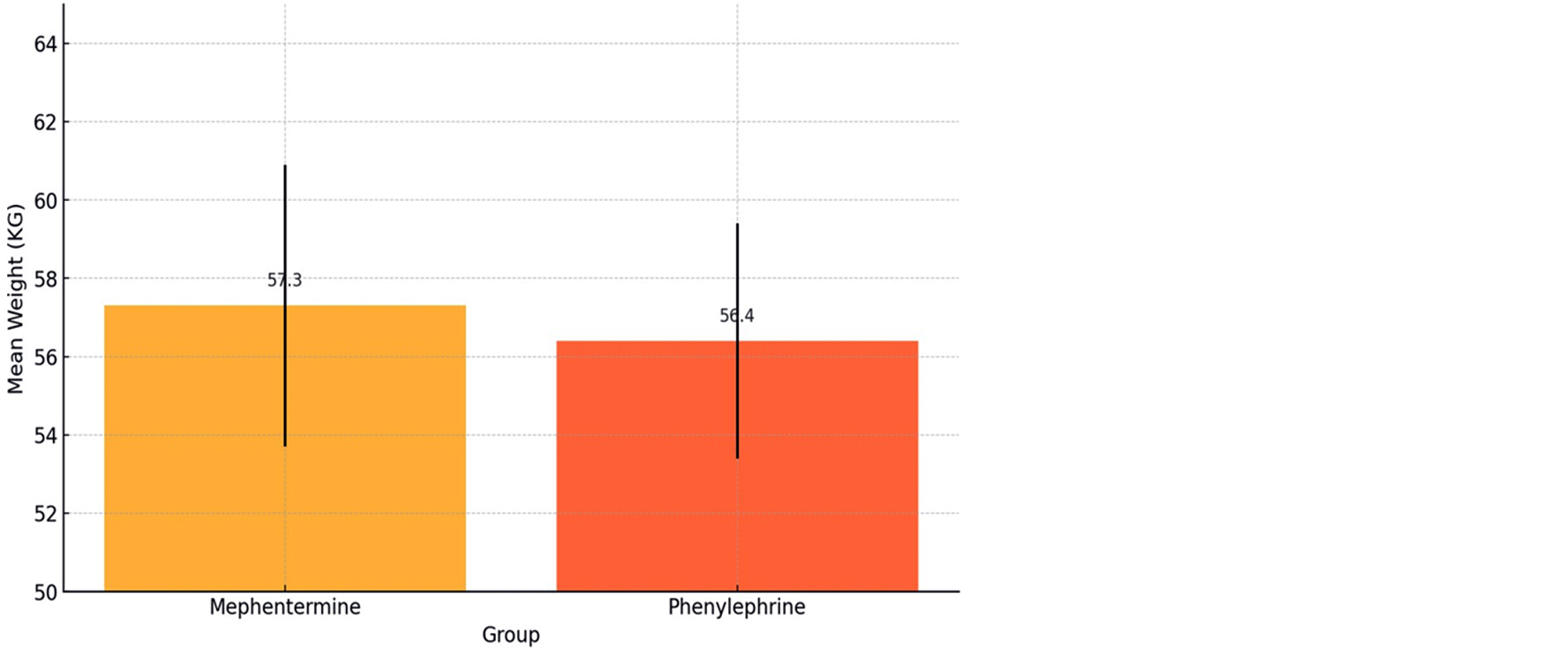
Figure 2: Distribution of mean weight of study subjects among the groups.
A detailed analysis of changes in heart rate, SBP, DBP and MAP of each patient was done, during a caesarean section under spinal anaesthesia. Hemodynamic data was compared between two groups who received mephentermine and phenylephrine. There was no significant difference was observed between the efficacy of phenylephrine and mephentermine on heart rate, SBP, DBP and MAP during LSCS. Significant hemodynamic changes began to emerge in the minutes following cord clamping between the two groups.
One minute after cord clamping, the groups who received mephentermine and phenylephrine had a mean heart rate of 75.6 bpm and 71.1 bpm, respectively. A significant p-value of 0.021 indicates superior performance of mephentermine in maintaining a higher heart rate. However, at 2-, 3- and 4-minutes post-clamping, both drugs showed equivocal results (p value 0.073, 0.076, and 0.08, respectively). After 5 minutes post-clamping, mephentermine and phenylephrine showed mean heart rate 76.6 bpm and 73.6 bpm, respectively with a statistical significance (p=0.045). Hence, the mephentermine group demonstrated an overall better performance in maintaining higher heart rate after cord clamping compared to the phenylephrine group (Table 1).
Table 1: Comparison of mean heart rate of study subjects at different time intervals among the groups.
|
Heart Rate (Bpm)
|
Group
|
Mean
|
95% Confidence Interval
|
SD
|
T value
|
P value
|
|
Lower
|
Upper
|
|
Pre op
|
B
|
84.5
|
81.5
|
87.5
|
9.5
|
0.6
|
0.54
|
|
A
|
83
|
80.5
|
85.5
|
9
|
|
after SAB
|
B
|
79.6
|
76.6
|
82.7
|
8.46
|
0.8
|
0.42
|
|
A
|
78
|
75.5
|
80.5
|
8.2
|
|
Just before cord clamping
|
B
|
75.6
|
72.6
|
78.7
|
8.46
|
0.7
|
0.49
|
|
A
|
74
|
71.5
|
76.5
|
8.1
|
|
At the time cord clamping
|
B
|
73.6
|
70.6
|
76.7
|
8.46
|
0.6
|
0.53
|
|
A
|
72
|
69.5
|
74.5
|
8
|
|
1min
|
B
|
75.6
|
72.6
|
78.7
|
8.46
|
2.38
|
0.021
|
|
A
|
71.1
|
68.7
|
73.5
|
6.68
|
|
2min
|
B
|
76.6
|
73.6
|
79.7
|
8.46
|
1.83
|
0.073
|
|
A
|
73.2
|
70.8
|
75.5
|
6.62
|
|
3min
|
B
|
78.6
|
75.6
|
81.7
|
8.46
|
1.81
|
0.076
|
|
A
|
75.2
|
72.9
|
77.6
|
6.5
|
|
4min
|
B
|
79.6
|
76.6
|
82.7
|
8.46
|
1.78
|
0.08
|
|
A
|
76.3
|
74
|
78.6
|
6.42
|
|
5min
|
B
|
76.6
|
73.6
|
79.7
|
8.46
|
1.64
|
0.045
|
|
A
|
73.6
|
71.4
|
75.8
|
6.13
|
One minute after cord clamping, the phenylephrine group had a mean SBP of 113 mmHg compared to mephentermine group who had a mean SBP of 108 mmHg, closely approaching statistical significance (p=0.06). By the end of 2-minutes post clamping, phenylephrine maintained higher SBP at 112 mmHg versus 110 mmHg for mephentermine, with statistical significance (p=0.031). This trend of phenylephrine maintaining a higher mean SBP continued at 3-minutes (p=0.058) and was again found to be statistically significant at 4-minutes (p=0.045) and at 5 minutes (p=0.001). Although, both phenylephrine and mephentermine effectively managed SBP during the surgery but overall phenylephrine demonstrated a better efficacy in maintaining higher SBP levels in the minutes following cord clamping (Table 2).
Table 2: Comparison of mean systolic blood pressure (mmHg) of study subjects at different time intervals among the groups.
|
SBP (mmHg)
|
Group
|
Mean
|
Lower CI
|
Upper CI
|
SD
|
T value
|
P value
|
|
Pre op
|
A
|
124
|
120
|
129
|
13.27
|
0.8
|
0.43
|
|
B
|
123
|
119
|
127
|
10
|
|
After SAB
|
A
|
119
|
115
|
123
|
11.52
|
0.9
|
0.36
|
|
B
|
118
|
114
|
122
|
10
|
|
Just before cord clamping
|
A
|
114
|
111
|
118
|
9.18
|
0.7
|
0.49
|
|
B
|
113
|
109
|
117
|
9
|
|
At the time of cord clamping
|
A
|
109
|
104
|
113
|
11.79
|
0.6
|
0.54
|
|
B
|
108
|
104
|
112
|
8
|
|
1min
|
A
|
113
|
109
|
117
|
11.48
|
1.926
|
0.06
|
|
B
|
108
|
104
|
112
|
7.5
|
|
2min
|
A
|
112
|
108
|
116
|
10.91
|
2.214
|
0.031
|
|
B
|
110
|
106
|
114
|
7
|
|
3min
|
A
|
115
|
111
|
119
|
7.1
|
-1.931
|
0.058
|
|
B
|
112
|
109
|
115
|
8.62
|
|
4min
|
A
|
117
|
114
|
120
|
8.52
|
2.046
|
0.045
|
|
B
|
116
|
113
|
119
|
8
|
|
5min
|
A
|
118
|
115
|
122
|
9.37
|
4.12
|
0.001
|
|
B
|
116
|
113
|
119
|
6
|
At 1minute post-clamping, the phenylephrine group had a mean DBP of 70 mmHg compared to mephentermine group who had a mean DBP of 65 mmHg, with statistical significance (p=0.016). Phenylephrine maintained a better efficacy in achieving a higher DBP with statistical significance at 3-minutes (p=0.049), 4-minutes (p=0.043) and at 5-minutes (p=0.021). Hence, phenylephrine demonstrated superior performance in maintaining higher DBP levels than mephentermine in the minutes following cord clamping (Table 3).
Table 3: Comparison of mean diastolic blood pressure (mmHg) of study subjects at different time intervals among the groups.
|
DBP (mmHg)
|
Group
|
Mean DBP
|
Lower CI
|
Upper CI
|
SD
|
T value
|
P value
|
|
Pre op
|
A
|
77.9
|
75.7
|
80.1
|
6.14
|
0.267
|
0.79
|
|
B
|
75
|
73
|
77
|
5.9
|
|
After SAB
|
A
|
72.8
|
70.5
|
75
|
6.22
|
1.685
|
0.097
|
|
B
|
70
|
68
|
72
|
5.5
|
|
Just before cord clamping
|
A
|
70.6
|
68
|
73.1
|
7.04
|
-0.019
|
0.985
|
|
B
|
68
|
66.3
|
69.7
|
4.4
|
|
At the time of cord clamping
|
A
|
68.7
|
65.8
|
71.5
|
7.93
|
0.104
|
0.918
|
|
B
|
66
|
64.4
|
67.6
|
4.5
|
|
1min
|
A
|
70
|
66.6
|
73.3
|
9.7
|
2.51
|
0.016
|
|
B
|
65
|
64.1
|
67.9
|
5
|
|
2min
|
A
|
70.5
|
67.2
|
72.7
|
8
|
1.97
|
0.054
|
|
B
|
67
|
66
|
70
|
5.5
|
|
3min
|
A
|
73
|
69.6
|
74.5
|
6.5
|
2.02
|
0.049
|
|
B
|
70
|
69
|
73
|
4.9
|
|
4min
|
A
|
74
|
70.7
|
75.4
|
5
|
3.76
|
0.043
|
|
B
|
70
|
70
|
74
|
3
|
|
5min
|
A
|
76
|
72.9
|
76.4
|
5
|
4.7
|
0.021
|
|
B
|
71
|
71.2
|
74.8
|
3
|
At 1-minute post-clamping, phenylephrine showed a MAP of 85 mmHg which is considerably higher than mephentermine (78 mmHg), with a statistically significant difference (p=0.002). The better performance of phenylephrine as compared to mephentermine in maintaining higher MAP, continued at 2-minutes (p<0.001), 3-minutes (p=0.0023) and 5-minutes (p<0.001), with MAP readings consistently higher at each of these time intervals. Overall, both drugs were found effective in managing MAP during the procedure but phenylephrine demonstrated a superior efficacy in providing better hemodynamic stability, particularly in the critical minutes following cord clamping (Table 4).
Table 4: Comparison of mean arterial pressure (mmHg) of study subjects at different time intervals among the groups.
|
MAP (mmHg)
|
Group
|
Mean MAP
|
Lower CI
|
Upper CI
|
SD
|
T value
|
P value
|
|
Pre op
|
A
|
92.8
|
90.2
|
95.3
|
7.02
|
1.603
|
0.114
|
|
B
|
90
|
88
|
92
|
6.5
|
|
After SAB
|
A
|
86.7
|
84.2
|
89.2
|
6.9
|
1.931
|
0.059
|
|
B
|
83.5
|
81.5
|
85.5
|
5.9
|
|
Just before cord clamping
|
A
|
84.5
|
81.6
|
87.4
|
10
|
1.234
|
0.224
|
|
B
|
82
|
78.5
|
81.5
|
4.8
|
|
At the time of cord clamping
|
A
|
81.6
|
78.3
|
85
|
9.1
|
1.925
|
0.061
|
|
B
|
78
|
76.5
|
79.5
|
4.7
|
|
1min
|
A
|
85
|
80.5
|
86.5
|
6
|
5.317
|
0.002
|
|
B
|
78
|
78
|
81.8
|
4
|
|
2min
|
A
|
87
|
81
|
87.1
|
6
|
5.84
|
<0.001
|
|
B
|
79
|
80.2
|
83.8
|
4.5
|
|
3min
|
A
|
88
|
83.6
|
88.7
|
5
|
5.98
|
0.0023
|
|
B
|
81
|
82.3
|
85.7
|
4
|
|
4min
|
A
|
85
|
80
|
85.4
|
6
|
2.02
|
0.048
|
|
B
|
82
|
83.2
|
86.8
|
5.5
|
|
5min
|
A
|
92
|
88.1
|
91.9
|
4
|
5.39
|
<0.001
|
|
B
|
86
|
87.2
|
90.6
|
4.6
|
Discussion
The present study found significant differences in heart rate between the mephentermine and phenylephrine groups at multiple time intervals. Before spinal anaesthesia (SAB), the mean heart rate in the mephentermine group was 84.5 ± 9.5 bpm compared to 83 ± 9.53 bpm in the phenylephrine group (p = 0.54), which was not statistically significant. After SAB, the heart rate was 79.6 ± 8.46 bpm for mephentermine and 78.7 ± 8.2 bpm for phenylephrine (p = 0.42), which also lacked significance. Although, significant heart rate changes were observed post clamping and it was observed that the phenylephrine group consistently exhibited lower heart rates than the mephentermine group. This suggests that mephentermine maintained higher heart rates during critical time after cord clamping. Sharma N et al. also reported concordant result, they have observed that phenylephrine was associated with an immediate peak effect (within 1–2 minutes) and a notable reduction in heart rate compared to mephentermine and ephedrine [10]. Results of study conducted by Chaturvedi N K, et al. also corroborated that heart rate significantly differ across groups after spinal anaesthesia (p < 0.05) [9].
The study also observed changes in SBP, DBP and MAP between the two groups at various point of time. Preoperatively, SBP in both the groups were comparable while post cord clamping, SBP was found to be higher in the phenylephrine group (119 ± 11.52 mmHg) as compared to the mephentermine group (118 ± 10 mmHg; p = 0.36). These results are consistent with the findings of Das et al. that also demonstrated lower SBP values in the mephentermine group at critical time points [11]. Both the groups experienced a drop in DBP post-SAB, just before, at the time of cord clamping as well as 4- and 5-minutes post-clamping. However, the mephentermine group showed an overall significantly lower DBP as compared to the phenylephrine group, suggesting a greater depressor effect of mephentermine on DBP. Das et al. reported a similar trend, where the phenylephrine group (72.6 ± 9.2 mmHg) showed significantly higher DBP than in the mephentermine group (67.8 ± 7.4 mmHg, p < 0.05) at 2 minutes post-administration [11]. Preoperative MAP values were similar between groups (phenylephrine: 92.8 ± 7.02 mmHg, mephentermine: 90 ± 6.5 mmHg). Despite the higher mean for phenylephrine, the difference was not statistically significant (p=0.114). At the time of cord clamping, phenylephrine maintained a MAP of 81.6 mmHg compared to mephentermine 78 mmHg, again nearing statistical significance (p=0.061). Significant differences emerged post-cord clamping.
At 1 minute, phenylephrine showed a MAP of 85 mmHg, considerably higher than mephentermine’s 78 mmHg, with a statistically significant difference (p=0.002). This pattern of higher MAP maintained by phenylephrine continued at 2 minutes (p<0.001), 3 minutes (p=0.0023), and 5 minutes (p<0.001), with MAP readings consistently higher for phenylephrine compared to mephentermine at each of these time points. Overall, while both drugs were effective at managing MAP during the procedure, phenylephrine demonstrated superior performance, particularly in the critical minutes following cord clamping. These findings are in line with those of Das et al., who recorded the lowest MAP after oxytocin infusion in their Phenylephrine group (75 mcg) as 72.50 ± 5.87 mmHg, compared to 67.80 ± 6.16 mmHg in another group, reinforcing Phenylephrine’s stabilizing effect on MAP [11]. Divyabharathi S et al also find that phenylephrine group had maintained systolic pressure, diastolic pressure and mean arterial pressure than mephentermine group [12]. The main limitation of this study is that it included only ASA grade II patients, which limits the findings of patients with different ASA grades or higher-risk populations. The methodology used a single prophylactic bolus dose of phenylephrine (75 mcg) and mephentermine (6 mg) without exploring other dosing regimens or continuous infusion techniques, which could limit the scope of comparison.
Conclusion
In conclusion, Mephentermine proved more effective in maintaining heart rate during critical periods, while Phenylephrine demonstrated superior efficacy in stabilizing systolic, diastolic, and mean arterial pressures following cord clamping. These findings highlight Mephentermine's advantage in heart rate support and Phenylephrine's consistent hemodynamic stability, particularly in blood pressure maintenance.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Patel HS, Shashank MR, Shivaramu BT. A comparative study of two different intravenous bolus doses of phenylephrine used prophylactically for preventing hypotension after subarachnoid block in cesarean sections. Anesth Essays Res. 2018; 12:381–385.
[2] Mohta M, Kumar V, Agarwal R, Chilkoti G, Duggal S. Efficacy of phenylephrine in preventing hemodynamic responses of oxytocin during elective cesarean section. Ann Natl Acad Med Sci (India). 2019; 55:48‒53.
[3] Sharkey AM, Siddiqui N, Downey K, Ye XY, Guevara J, et al. Comparison of intermittent intravenous boluses of phenylephrine and norepinephrine to prevent and treat spinal-induced hypotension in caesarean deliveries: randomized controlled trial. Anesth Analg. 2019; 129:1312–1318.
[4] Hasanin A, Amin S, Refaat S, Abd Alaziz WE, Elsayed M, et al. Norepinephrine versus phenylephrine infusion for prophylaxis against post-spinal anaesthesia hypotension during elective caesarean delivery: a randomised controlled trial. Anaesth Crit Care Pain Med. 2019; 38:601–607.
[5] Chaturvedi NK, Panigrahi MR, Mukhopadhyay B. Efficacy and safety of intravenous phenylephrine and mephentermine for management of hypotension during spinal anaesthesia. Indian J Clin Anaesth. 2020; 7:177‒181.
[6] Shah PJ, Agrawal P, Beldar RK. Intravenous norepinephrine and mephentermine for maintenance of blood pressure during spinal anaesthesia for caesarean section: an interventional double-blinded randomised trial. Indian J Anaesth. 2020; 64:S235–S241.
[7] Hiruthick S, Sanjana KVL. Clinical comparative study to compare the effect of two different doses of phenylephrine on spinal induced hypotension during caesarean section. J Pharm Res Int. 2021; 33:482–489.
[8] Rai AV, Prakash S, Chellani H, Khurana S, Gupta S, et al. Comparison of phenylephrine and norepinephrine for treatment of spinal hypotension during elective cesarean delivery - a randomised, double-blind study. J Anaesthesiol Clin Pharmacol. 2022; 38:445–452.
[9] Chaturvedi NK, Panigrahi MR, Mukhopadhyay B. Efficacy and safety of intravenous phenylephrine and mephentermine for management of hypotension during spinal anaesthesia. Indian J Clin Anaesth. 2020; 7:177‒181.
[10] Sharma N, Agarwal S, Modi YC, Yadav A, Yadav J, et al. Effect of two different doses of intravenous phenylephrine on the prevention of oxytocin induced hypotension in lower segment caesarean section under subarachnoid block: a randomised controlled study. J Clin Diagn Res. 2023; 17:UC16–UC21.
[11] Das S, Potli S, Madhusudhana R, Krishnamurthy D. A comparative study of phenylephrine, ephedrine and mephentermine for maintenance of arterial pressure during spinal anaesthesia in caesarean section. IOSR J Dent Med Sci. 2015; 14:80–85.
[12] Divyabharathi S, Devi N, Kumar M, Ramesh K, Lakshmi P, et al. Mephentermine vs. phenylephrine for prevention and management of maternal hypotension during caesarean section under spinal anaesthesia and their effects on foetal outcome - a randomised control trial. J Clin Diagn Res. 2022; 16:9–13.
[13] Kumar PS, Lokesh P, Karunakar B. A comparative study of bolus phenylephrine and mephentermine for treatment of hypotension during spinal anaesthesia for caesarean section. Int J Med Anesthesiol. 2020; 3:93–99.