Full Text
Introduction
Cerebrovascular diseases caused 200,000 deaths each year in the United States and are a major cause of disability [1]. Stroke (Cerebrovascular diseases) is one of the leading causes of death and disability in India. The estimated adjusted prevalence rate of stroke ranges from 84-262/100,000 in rural areas and 334-424/100,000 in urban areas. The incidence rate is 119-145/100,000 based on the recent population-based studies. There is also a wide variation in case fatality rates, with the highest being 42% in Kolkata [2]. The risk factors identified were hypertension alone in 40%, hypertension with diabetes in 25%, and hypertension with other risk factors (raised cholesterol, ischemic heart disease) accounted for another 20%. Diabetes and ischemic heart disease alone were present in 5% of cases. Platelets are cytoplasmic fragments of bone marrow megakaryocytes, with a diameter of 3-5 μm and a volume of 4.5–11 fL. Thrombosis is a critical event in the arterial diseases associated with myocardial infarction and stroke. Platelet indices like platelet count, mean platelet volume (MPV), platelet distribution width (PDW), platelet to large cell ratio (P-LCR) & plateletcrit (PCT) reflect the level of platelet function and activation.
Platelet Indices: Platelets are heterogeneous regarding their size, density and haemostatic potential. Platelet size (MPV) is a marker (and possibly determinant) of platelet function, large platelets being potentially more reactive. PDW is a measure of platelet anisocytosis & combined use of MPV and PDW could predict activation of coagulation more efficiently. P-LCR measures the number of platelets falling above the 12fl threshold on the platelet size histogram divided by the total number of platelets. It has also been used to monitor platelet activity.
Platelet count and platelet indices in the blood can be rapidly measured using an automated haematologic analyser. Platelet indices, being biomarkers of platelet activation, give an insight into the pathological process before an acute event like ischemic stroke and also have prognostic implications. So, platelet count and platelet volume indices are an important, simple, effortless, and cost-effective tool that can be used for predicting the possibility of impending acute events like stroke, especially in countries such as India. It also helps in implementation of newer therapeutic strategy in future to reduce the risk of ischemic stroke in an individual with risk factors for stroke as well as recurrence of acute events.
The change in platelet count in cases of acute ischaemic stroke in comparison to the control group were studied. The changes in platelet indices like MPV, PDW, PDW, PCT in cases of acute ischemic stroke in comparison to control group were investigated.
Materials and method methods
This is an observational, case-control study. The study was conducted after approval from the institutional ethic committee. The cases admitted in indoors of general medicine ward of North Bengal medical college and hospital with symptoms suggestive of acute stroke and confirmed radio-logically by CT scan or MRI of the brain as having acute ischemic stroke and age and sex matched with healthy controls were selected from April 2019 to March 2020.
Inclusion criteria: Patients with acute ischaemic stroke (fulfilling the clinical and radiological criteria of stroke), aged 18 years or above and willing candidates were considered as case. Age and sex matched healthy subjects with no history of ischemic stroke were included as controls. They were aged 18 years or above and those who gave consent.
Exclusion criteria: Patients with haemorrhagic stroke, history of cardio-embolic stroke and any co-morbid condition that may alter platelet function were excluded from the study group.
Study tools: Pre-designed questionnaire schedule, sphygmomanometer, stethoscope, hammer, torch etc., disposable syringes with needle, cotton, spirit, tourniquet and EDTA containing vial and plain vial, gloves, needle destroyer were gathered. Laboratory equipment like Binocular compound microscope, glass slides, Leishman stain, automated cell counter (Sysmex XS-800i), Haemocytometer (improved Neubauer Chamber) and 1% aqueous ammonium oxalate as diluent for platelet count and automated analyser were used for the study purpose.
Statistical analysis
The collected data was organized and entered in the microsoft excel data sheet. The student’s t test is applied for comparison of mean value & data was analysed using SPSS.
Results
The following results were obtained after analysing the collected data. A total of 156 subjects (case-78, control-78) were studied, 88 of which were male and 68 were female subjects. The mean age of study subject was 61.22 years with range from 41 years to 90 years. Mean age of case and control group. The mean age of the cases was 61.58 years and mean age of control was 60.86 years. The age range for the 78 cases- 41-90 years (Figure 1). Mean age for cases- 61.58 years. The majority of the cases are in the 61-70 years age group (38.46%). Distribution of cases according to history of previous stroke. Among the 78 patients, only 2 patients had previous h/o ischaemic stroke. Distribution of cases was according to type of infarct. Among the 78 patients, 51 patients had cortical infarct (65.38%), 27 patients had lacunar infarct (34.62%).
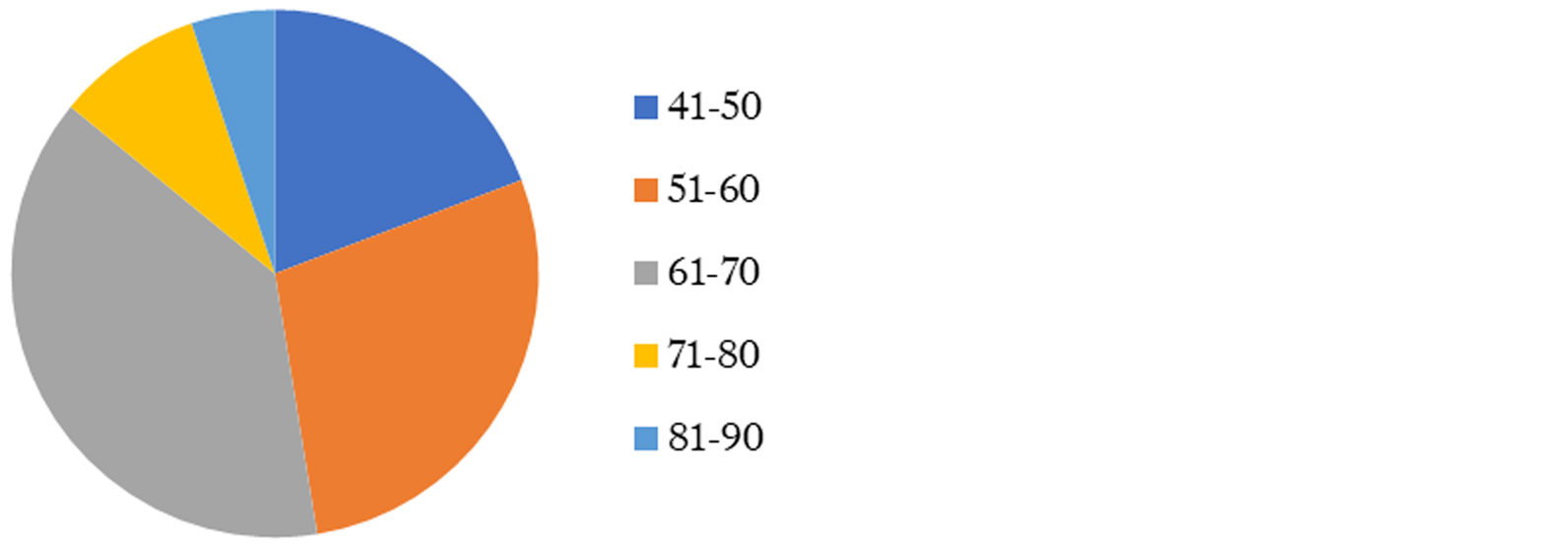
Figure 1: Age distribution of study subjects.
MPV value of cases and controls: MPV value of cases: Mean-12.25 fl, SD-1.01fl. MPV value of control: Mean- 10.42fl, SD-0.92 fl. There is significant higher value of MPV in cases than control subjects (p=0.00, CI- 95%). Mean platelet counts of cases and control subjects. Platelet count of cases: Mean-227589.7 cells/micro-liter, SD-62642.7 cells/micro-liter. Platelet count of control: Mean-280500 cells/micro-liter, SD-70210 cells/micro-liter. There is significantly higher platelet count in control group (p=0.000) than case (CI-95%). Mean PDW of cases and control subject. Mean PDW of cases: 17.69 fl, SD- 3.22 fl. Mean MPV of cases and control subjects. Mean PDW of control group: 13.67 fl, SD- 3.15 fl. PDW was significantly increased in cases in comparison to control group, p value- 0.00 (p value <0.05 is considered as significant, CI- 95%). Mean PLCR (%) of case and control subject. Mean P-LCR of cases – 42.19%, SD- 8.77%. Mean P-LCR of control subjects- 28.66%, SD-7.26%. So, cases have significantly higher P-LCR values than control subjects (p value- 0.00, CI- 95%). Mean PCT of cases-were 0.27%, SD-0.07% and mean PCT of control subjects-were 0.29%, SD- 0.07%. Difference between mean PCT of cases and control subjects is not statistically significant-P value- 0.26 (> .05, CI- 95%).
Platelet morphology among the cases (ischemic stroke patients) were among the cases (n=78), large platelets were found in peripheral blood smear in 36 patients (46.15%), platelet clumps found in 29 patients (37.17%) (Figure 2). Among the 36 patients having large platelet, 17 patients (47.22%) also have platelet clumps in peripheral blood smear. MPV value of cases was according to the age group. Among the cases, mean MPV value is highest in the 41–50-year age group (12.37fl), lowest in the 81–90-year age group (12.1fl) (Table 1).
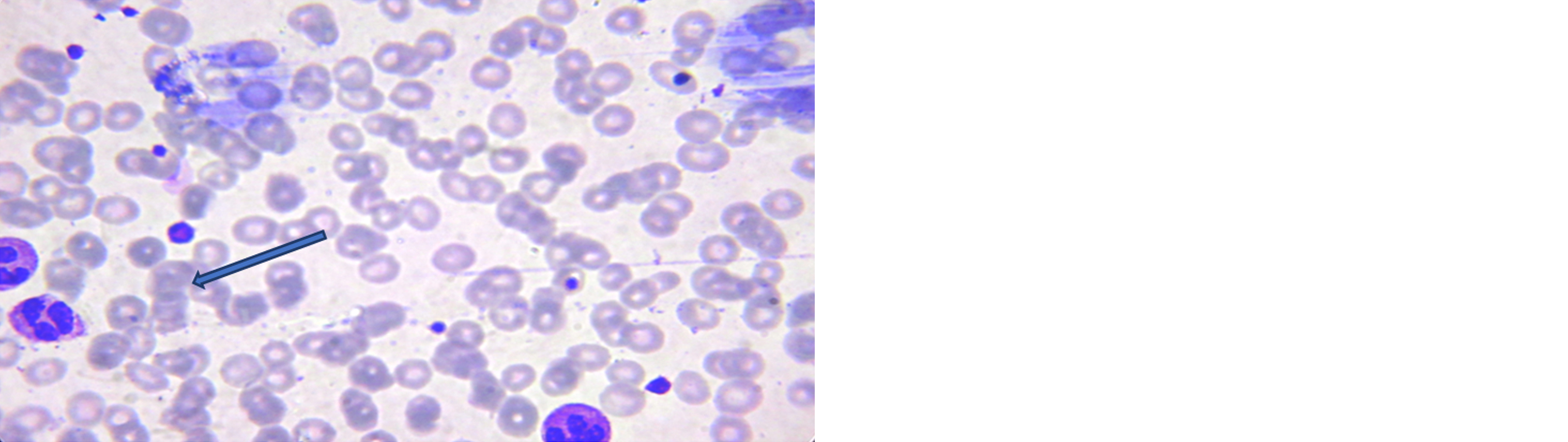
Figure 2: PBF showing large platelet (arrow).
Table 1: MPV value of cases according to age group.
|
AGE (Years)
|
MPV (fL)
|
|
41-50
|
12.373
|
|
51-60
|
12.136
|
|
61-70
|
12.27
|
|
71-80
|
12.342
|
|
81-90
|
12.1
|
Table 2: Mean MPV of cases and control subjects.
| |
Mean MPV (Fl)
|
|
Case
|
12.25
|
|
Control
|
10.42
|
In the present study, we found the mean MPV value of cases is 12.25 fl with a SD of 1.01fL. The mean MPV value of control is 10.42fl with a SD of 0.92 fl. There is a statistically significant higher value of mean MPV in cases than in control subjects (p=0.00, CI- 95%)(Table-2). The mean platelet count of cases is 227590 cells per micro-liter with a SD of 62643cells per micro-liter and the mean platelet count of control is 280500 per micro-liter with a SD of 70210 (Table 3). The mean platelet count of cases is lower than the control group which is statistically significant (p=0.000, CI-95%).
Table 3: Mean platelet count of cases and control subjects.
| |
Mean platelet count per cmm
|
|
Case
|
227589.7
|
|
Control
|
280500
|
Discussion
Stroke is one of the leading causes of death and disability in India. The estimated adjusted prevalence rate of stroke ranges, 84-262/100,000 in rural areas and 334-424/100,000 in urban areas. The incidence rate is 119-145/100,000 based on the recent population-based studies. There is also a wide variation in case fatality rates, with the highest being 42% in Kolkata.
In the present study, mean age of cases is 61.58 years with a range of 41-90 years. The mean age of control is 60.86 years with a range of 42 -88 years. Both groups include 44 male and 34 female subjects. So, there is male predominance (56%) among the ischaemic stroke cases. Most of the study subjects are in the 61–70-year age group (38.46% of cases and 37.18% of control subjects). The result is similar to other studies of stroke conducted in India. In a study conducted by Priyanka Meena et al, the mean age of the study group was 54.85 ±11.85 yrs. (range 31 to 76 yrs.) with male predominance [3]. The mean age and gender distribution of the present study is also similar to the study conducted by Parvaiz. A. Shah et al. where they found the mean age of the ischemic stroke was 58 years (range 34 to 78 years). Males comprised 59% of the study group. Among the cases, 51 patients have cortical infarct and 27 patients have lacunar infarct, 45 patients (57.70%) have a history of hypertension, 29 patients (37%) have h/o current smoking and only 2 patients have a previous history of ischaemic stroke. Among the control group 17 subjects (21.79 %) have a history of hypertension and 19 subjects (24%) have h/o current smoking.
In the present study, most common clinical presentation of cases is hemiparesis, other clinical presentations are aphasia, dysarthria, unconsciousness, facial weakness etc. This finding is also supported by the studies done by Kaul S et al & Md. Abu Naser Siddique et al. In the present study, we found the mean MPV value of cases is 12.25 fL with a SD of 1.01fL. The mean MPV value of control is 10.42fL with a SD of 0.92 fL. There is statistically significant higher value of mean MPV in cases than in control subjects (p=0.00, CI- 95%). The mean platelet count of cases is 227590 cells per micro-liter with a SD of 62643cells per micro-liter and the mean platelet count of control is 280500 per micro-liter with a SD of 70210. The mean platelet count of cases is lower than the control group which is statistically significant (p=0.000, CI-95%). The result of our study is similar to other studies in the literature. Butterworth RJ et al found in their study that MPV was significantly higher in patients with ischaemic stroke than the control group: mean (SD) 7.35 (1.05) vs 7.09 (0.74) fL, 2 p=0.04. But they found no difference in platelet count between ischaemic stroke patients and controls. Patients who were dead or dependent at 3 months had a significantly higher baseline MPV and a tendency to a lower platelet count than those who returned to independence.
In another study conducted by O’Malley T et al over 58 stroke patients who were consecutively admitted to a geriatric medical unit. Platelet indices were calculated in two settings: acute CVA (< 48 h) and chronic (> 6 months) and matched with control platelet indices. The study found mean platelet volume was higher in acute stroke (11.3 compared with 10.1 fL in control subjects; p< .001, Student's t test). In addition, platelet count was reduced in stroke patients (255 x 10(9)/L) compared with control subjects (299 x 10(9)/L; p < .01). In a study conducted by Neki N.S. et al, also displayed a statistically significant correlation with ischemic stroke with MPV (p value of 0.000). Average MPV were 8.92±1.03fl compared to controls in which the average was 7.67±1.38fl [4]. Platelet count, found in acute stroke was remarkably lower in comparison to control study (213611+/- 65652 per micro-liter vs. 29952+/- 60611 per micro-liter, p< 0.001). PLC reached the normal on and after 9th day. The mean platelet volume was significantly greater than in the controls (11.26fL +/-1.29 fl vs. 8.93 fl+/- 0.93 fl, p< 0,001) and normalization generally occurs on the forty-fifth day. Studies conducted in our country also had similar results. Meena et al performed a hospital based cross sectional study which showed a statistically significant higher MPV value in cases than controls subjects 11.88 (9.5 to 14.5) and 9.72(7.6 to 13.2) respectively. When MPV and total platelet count were compared in patients, an inverse correlation was seen in the MPV values and mean platelet count (r=-p < 0.01) by using Pearson’s correlation coefficient [3].
In the present study, mean PDW (platelet distribution width) of cases is 17.69 fl with a SD of 3.22 fl and means PDW of the control group is 13.67 fl with a SD of 3.15 fl. PDW is significantly increased in cases compared to the control group (p=0.00, CI- 95%). In the present study, also shows a statistically significant (p=0.00, CI-95%) higher value for mean P-LCR in cases compared to control group (mean P-LCR of cases is 42.19% with a SD of 8.77%and mean P-LCR of control subjects is 28.66% with a SD of 7.26%).There is statistically nonsignificant (p=0.26, CI-95%) changes in value of PCT among cases and control group (mean PCT of cases is 0.27% with a SD of 0.O7% and the mean PCT of control subjects is 0.29% with a SD of 0.07%). The mean haemoglobin of cases is 11.97 g/dl with a SD of 1.83 g/dl and mean haemoglobin of control subjects is 12.33 g/dl with a SD of 1.41 g/dl (p=0.98, CI95%). The mean total leukocyte count of cases is 9932 cells /micro-liter while the mean TLC of control subjects is 7920 cells/ micro-liter. The value of TLC of cases is significantly higher than in control subjects (P value- 0.00, CI- 95%) which may be due to stress induced leucocytosis in patients with acute stroke.
In a study conducted by Pandey et al., they found with cerebrovascular disease patients, MPV was 10.30±0.83fL, PDW was 14.50±0.55 fL, platelet count was 260×109 ± 29×109/L while in control MPV was 8.14± 0.72 fl, PDW was 10.71±0.48 fl, platelet count was 285×109 ± 50 ×109/L. MPV and PDW were higher and platelet count lower in the cerebrovascular disease group and a highly significant difference (p<0.001) was found on comparing with controls [5]. In a study conducted by Waseem Al-Tameemi et al., they found mean platelet count (MPC) differs significantly in cases of multiple strokes in comparison with those having first stroke or the control group, while no statistically significant differences were reported with the other indices (MPV, PDW or P-LCR). In the present study, platelet morphology was observed in peripheral blood smear and the presence of large platelet and platelet clumps are also observed. Larger platelets are seen in the peripheral blood smear of 36 ischemic stroke patients (46.15%) and platelet clumps were found in the peripheral blood smear of 31 ischemic stroke patients (37.18%). Among the 36 patients having larger platelets in peripheral blood, platelet clumps were found in 17 cases (47.22%). No similar study is available in literature that observed platelet morphology in peripheral blood smear under light microscopy.
There is statistically significant (p=0.00) higher MPV value in cases with cortical infarct (mean MPV 12.53 fl with a SD of 0.98 fl) than cases with lacunar infarct (mean MPV 11.71 fL with a SD of 0.84 fl). Statistically significant higher value observed in PDW (18.5fl vs 16.16fl, p=0.004) and PLCR (44.84% vs 37.18%, p=0.001) among patients with cortical infarct than lacunar infarct and there is statistically insignificant higher mean platelet count (226059 cells/micro-liter vs 230481cells/micro-liter, p=0.93) in lacunar infarct cases than cortical infarct cases and PCT% (0.28 vs 0.27, p=0.27) is higher in patients with cortical infarct than lacunar infarct. In the present study, patients with lacunar infarct also have statistically significant higher mean value of MPV (11.71 fl vs 10.42 fl, p=0.00), PDW (16.16flvs 13.67fl, p=.00), PLCR (37.18% vs 28.66%, p=0.00), and lower platelet count (230481 cells/ micro-liter vs 280500 cells/ micro-liter, p=0.00) than control subjects. Differences between mean PCT of lacunar infarct and control subjects is statistically nonsignificant (0.27% vs 0.28%, p>0.05).
Pikija et al also discovered that higher MPV was linked with greater infarct size [estimate 0.259, 95% confidence interval (CI) 0.004-0.513, p=0.046], higher risk of morbidity and morbidity at 7 days of CVA [relative risk (RR)=1.077, 95% CI 1.005-1.115, p=0.036], as well as 3 months after CVA (RR=1.077, 95% CI 1.001-1.158, p=0.048). Butterworth RJ et al also had similar outcome in their study. MPV was significantly higher in patients with ischaemic stroke than the control group: mean (SD) 7.35 (1.05) vs 7.09 (0.74) fl, 2 p=0.04; they also found that MPV was higher in patients with cortical stroke: 7.46 (1.00) fl, 2 p=0.039, but not lacunar infarction: 7.14 (1.16) fl, 2 p=1.0. No difference was seen in PC between ischaemic patients and controls: 231 (82) 10(9)/l vs 236 (54) 10(9)/l, 2 p=0.63. Increased platelet volume seen in acute ischemic CVA and that remain elevated even at 3 months after stroke. This findings were mainly confined to cortical CVA-infarction cases with the habit of current smoking have a statistically significant higher value of mean MPV (12.62fl vs 10.03fl, p=0.01), mean PDW (19.042fl vs 16.886fl, p=0.00) and mean PLCR (45.67% vs 40.14%, p=0.00) than cases without habit of current smoking, while non-significant higher mean platelet count (220862/micro-liter vs 231571/micro-liter, p=0.01) & mean PCT (0.275% vs 0.276%, p=0.59) are found in cases with no history of current smoking. The cross-sectional study conducted by Swaminathan et al had similar results which showed significantly high values of MPV, and PDW (P<0.05) among smokers compared to nonsmokers. MPV, PDW, and P-LCR were found to be positively associated with the intensity of smoking, pack-year, and duration of smoking [6]. In the present study, there is nonsignificant higher value of mean MPV (12.30 fl vs 12.18fl) but lower mean platelet count (226432/microliter vs 229088/micro liter) among ischaemic CVA patients with h/o HTN (45 cases) than cases without h/o HTN (33 cases). Differences between mean PDW (17.78 fl vs 17.58 fl), PLCR (40.40 % vs 40.03%), PCT (0.27% vs 0.28%) values are also statistically nonsignificant (p value > 0.05) between these two groups. In a study conducted by Meena et al., MPV has been compared with the various risk factors for stroke. They found that MPV was higher in patients with stroke and diabetes mellitus with a suggestive significance (p<0.001) when compared to controls. (Mean MPV of cases-12.05fl & controls 9.62fl). But they found no statistical significant changes in platelet count and MPV with other risk factors like HTN, smoking, alcohol consumption etc [3]. Predictable correlation has been established between platelet indices and stroke [7]. The MVP index can be a marker of the type of stroke [8]. Significant correlation between Platelet lymphocyte ratio and NIHSS scores has been demonstrated by Govind et al. But they failed to demonstrate correlation between Platelet indices and NIHSS score [9]. Higher MPV was seen in ischemic stroke and lower platelet count was demonstrated both ischemic and hemorrhagic strokes as per Sadeghi et al [10]. As per the study of Li et al., there is evidence of a potential correlation between platelet crit and increased risk of stroke, confounded by blood pressure [11]. MPV was an independent predictor of poor short-term outcome of acute stroke after controlling for con-founders like diabetes.
Limitations of this study: single centre-based and over a limited time period, the study sample is small. The follow up of the patients was not done. Platelet functional studies are also needed to correlate the findings with platelet functional status,
Conclusion
This single centre based observational study with case control design involving a total of 156 subjects (78 cases and 78 controls) has shown a statistically significant higher mean value of MPV, PDW & P-LCR and a lower mean value of platelet count in acute ischemic stroke patients than age & sex matched control subjects. In the present study, we also observed the platelet morphology in peripheral blood smear which requires further studies in the future and correlation with electron microscopic findings and platelet functional studies. Among the cases (ischemic stroke patients), patients with cortical infarct have significantly higher mean values of MPV, PDW and PLCR than patients with lacunar infarct. So, as larger platelets are haemostatic ally more active, their presence is probably a risk factor for developing thrombosis. Patients with larger platelets can easily be identified during routine haematological analysis. Hence, these indices serve as an important and cost-effective tool in predicting an impending ischemic event and can be used in the future, especially in resource poor countries like India. Further trials are required to explore the role of drugs, which may change the platelet morphology so that we can have a new line of preventive treatment for thrombotic events.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Smith WS, English JD, Johnson SC. Cerebrovascular diseases. Harrison‘s principles of internal medicine. Ed. Fauci AS, Braunwald E , Kasper DL, Hauser SL, Longo DL, Jameson JL et al 17th ed. Mc GrawHill; 2:2513–2535.
[2] Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013; 15:128–134.
[3] Meena P, Khare M, Airun A, Manohar, Saxena A. A study of platelet indices in patients of acute ischemic stroke: a prospective study. IOSR J Dent Med Sci. 2017; 16:26–29.
[4] Neki NS, Minda N, Jain A. A study of association of mean platelet volume and ischaemic stroke. Asian Pac J Health Sci. 2016; 3:212–219.
[5] Pandey M, Banthia BL, Sharma D, Rishi JP, Syed T, et al. A study of platelet volume indices in patients of ischaemic cerebrovascular disease. Ann Int Med Den Res. 2016; 2:90–93.
[6] Swaminathan A, Amitkumar K, Ganapathy S, Ayyavoo S. Evaluation of the impact of cigarette smoking on platelet parameters. National J Physiol Pharm Pharmacol. 2015; 5:426–430.
[7] Rajakumar I, Vidya TA, Ramachandran K, Hussain A, Aarthi J, et al. Platelet indices as prognostic markers of ischemic stroke and their correlation with lipid profile. Clin Neurol Neurosurg. 2024; 237:108119.
[8] Zarmehri B, Shahi B, Rahmani S, Tafti FD, Foroughian M. Association of platelet count and mean platelet volume (MPV) index with types of stroke. Caspian J Intern Med. 2020; 11:398–402.
[9] Govind D, Rao MM, Sudheer K. 2020. “A Study on the Correlation Between Platelet Indices and Severity Score in Acute Ischemic Stroke”. Int J Med Res Rev. 2020; 8:363–368.
[10] Sadeghi F, Kovács S, Zsóri KS, Csiki Z, Bereczky Z, et al. Platelet count and mean volume in acute stroke: a systematic review and meta-analysis. Platelets. 2020; 31:731–739.
[11] Li Y, Xiang W, Xue H, Meng T, Zhang T, et al. The impact of platelet indices on ischemic stroke: a Mendelian randomization study and mediation analysis. Front Neurol. 2023;
14. Available from: https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1302008