Abstract
Background: Pseudoexfoliation (PEX) syndrome, an age related microfibrillopathy having varied prevalence and associated with dense cataract, poorly dilating pupil resulting in challenging cataract surgeries. The present study aimed to evaluate pseudoexfoliation syndrome in eyes undergoing cataract surgery in tertiary care centre of Uttarakhand.
Materials and methods: A hospital based prospective study carried out from January 2021 to June 2022 and approved by the Institutional Ethical Committee. A total of 1000 eyes of 1000 patients to be operated underwent complete ophthalmic evaluation including refraction, tonometry, gonioscopy, slit lamp biomicroscopy for presence of pseudoexfoliation, cataract grading, and fundus examination. Patients with PEX were diagnosed and data analysed.
Results: A total of 54 PEX cases were diagnosed with 29 (53.7%) males and 25(46.3%) were females having mean age of 67.48 + 9.79 years, mean CCT was 528.46 + 18.49 micron and mean IOP was 19.81 + 5.88 mmHg. Prior to cataract surgery, an IOP of more than 21 mm Hg was noted in 40.7% (n=54) of pseudoexfoliative eyes. PXM on pupillary margin present in 51 (94.4%), on anterior lens capsule in 37 (68.5%), on iris in 31 (57.4%), on cornea in 5 (9.3%), phacodonesis in 6 (11.1%), Iris transillumination defect in 3 (5.6%), PXM on trabecular meshwork in 24 (44.4%) and sampaolesi line in 13 (24.1%).
Conclusion: PEX presents challenges that necessitate thorough preoperative planning for a safe surgery and a satisfactory postoperative result. Therefore, dilated anterior segment evaluation should be emphasised in daily practise to avoid early PEX patients from being undiagnosed.
Keywords: cataract; PEX; pseudoexfoliative; phacodonesis; sampaolesi line
Full Text
Introduction
Pseudoexfoliation (PEX) is defined as age related microfibrillopathy with deposition of dandruff like grayish white fibrillary material deposition on anterior segment of eye classically found on pupillary margin, iris, anterior lens capsule, trabecular meshwork and cornea. First description of PEX syndrome was given by Lindberg in 1917 and Alfred Vogt in 1925 describe PEX as remanent of pupillary membrane on anterior capsule of lens [1, 2]. Georgina Dvorak-Theobald in 1954 described the histochemical differences between pseudoexfoliative and true exfoliative materiel [3]. Pseudoexfoliation syndrome has multiple etiopathogenesis which are influenced by geographical and environmental factors. Genetic inheritance of pseudoexfolation syndrome has been documented having strong association with lysyl oxidase -like 1 (LOX L1) gene mutation resulting in abnormal overproduction of elastic microfibrillar components like fibrillin-1 [4].
PEX syndrome is easily identified by the presence of white flaky debris on the pupil margin and lens capsule. On full pupil dilation characteristic 'three-ring sign' on anterior lens capsule may present, consisting of a homogeneous centre zone of PXM deposition and a granular outer zone separated by a clear zone. PEX syndrome also presents with endothelial pigmentations and krukenberg’s spindles, iris ruff atrophy and transillumination defect, sampaolesi line pigmentation on trabecular meshwork. PEX syndrome is associated with secondary glaucoma, phacodonesis, corneal endothelial decompensation [5], iridodialysis, extension of rhexis, zonular dialysis and posterior capsular rent and postoperative like capsular phimosis and opacification [6]. Fibrillary material with composition similar to that of Pseudoexfoliation has been found on other visceral organs suggesting PEX syndrome may be ocular presentation of systemic disorder [7].
Pseudoexfoliation patients have greater risk for developing glaucoma and it is documented as most prevalent cause for secondary glaucoma [8-10]. Wide difference in prevalence of Pseudoexfoliation syndrome worldwide is reflective of complex factors involved in pathogenesis of Pseudoexfoliation syndrome [11]. Survey from Scandinavian countries shows higher prevalence of PEX syndrome as compared to Asian countries [12, 13]. PEX prevalence was reported to be 3.8%, 4.5%, 3.01% in South India [14-16]. Krishna das et al in 2003 reported a prevalence of 6 % [17]. Prevalence of Pseudoexfoliation increases with age without significant gender difference [5, 14, 18]. Some studies reported male predilection for PEX [15, 19]. In unilateral PEX patients, PXM has been detected on lens capsule or conjunctival sample of other eye on electron microscopy and a significant proportion of unilateral PEX showed conversion to bilateral disease [20, 21].
The aim of the present study was to evaluate the distribution of Pseudoexfoliation syndrome in eyes undergoing cataract surgery, cataract morphology and intraoperative complications.
Materials and methods
A hospital based prospective study was conducted in 1000 patients admitted for cataract surgery in the ophthalmology department of Shri Guru Ram Rai Institute of Medical and Health Sciences (SGRRIM&HS), Dehradun, Uttarakhand from January 2021 to June 2022. The ethical committee of SGRRIM&HS approved this research, and written consent was obtained from all the participants after explaining the protocol of the study. A total of 1000 eyes of 1000 patients aged 40 years and above diagnosed for senile cataract and admitted for cataract surgery were enrolled for the study. Patients with history of ocular trauma, congenital ocular abnormalities, previous history of ocular surgery or laser were excluded from the study. Uncorrected and best corrected vision was taken with Snellen chart. IOP measurement was done by Goldmann’s Applanation Tonometry. Assessment of ‘Angle of Anterior Chamber’ using Goldmann two mirror gonioscope and Shaffer system of grading angle width. Angles were evaluated for presence of pseudoexfoliative material and sampolesi’s line. Central corneal thickness using specular microscopy using the automated non-contact specular microscope Nidek CEM-530. By slit lamp biomicroscopy complete anterior segment examination was performed before and after pupil dilation. PEX syndrome was diagnosed by the presence of dandruff- like fluffy granular material on ocular structures like lens capsule, pupil margin, cornea, trabecular meshwork. Type of cataract and maximum pupillary dilatation by slit lamp biomicroscopy was recorded. Fundus evaluation was done by indirect ophthalmoscopy.
Statistical analysis
Microsoft excel was used for data entry and analyses were done using the Statistical Package for Social Sciences (SPSS) software. Descriptive statistics such as mean and standard deviation (SD) for continuous variables, frequencies and percentages were calculated for categorical Variables were determined and represented in tabular form. Difference in the two groups was tested for Statistical Significance and categorical variables tested by chi square test. P-value less than 0.05 considered to be statistically significant.
Results
1000 patients admitted for cataract surgery in a period of eighteen months were evaluated for presence of pseudoexfoliation syndrome, a total of 54 patients were diagnosed as case of pseudo exfoliation.
Mean age in PEX patients was 67.48 + 9.79 years while mean age in Non PEX patients was 63.39 + 9.73 years. The difference between these two were statistically significant (p value 0.003). Mean Central corneal thickness (CCT) in PEX patients was 528.46 + 18.49 micron and mean CCT in non PEX patients was 529.42 + 16.96 micron (p value 0.688) (Table 1).
Table 1: Baseline evaluation.
|
Parameters
|
Total patient
N =1000
|
Non PEX Pt.
N = 946
|
PEX Pt.
N= 54
|
p value
|
|
Age (Year)
(mean+ SD)
|
63.6 + 9.8
|
63.39 + 9.73
|
67.48 + 9.79
|
0.003
|
|
CCT (micron)
(mean+ SD)
|
529.4 + 17
|
529.42 + 16.96
|
528.46 + 18.49
|
0.688
|
|
IOP (mmHg)
(mean+ SD)
|
15.6 + 3.8
|
15.37 + 3.56
|
19.81 + 5.88
|
0.001
|
Abbreviations: CCT: Central corneal thickness, IOP: Intraocular pressure
Mean baseline intraocular pressure (IOP) in PEX patients was 19.81 + 5.88 mmHg while in non PEX patients mean IOP was 15.37 + 3.56 mmHg (p value 0.001). From 54 patients with PEX, 32 (59.3%) patients had IOP less than 21mmHg. 20 (37%) patients had IOP between 22-29mmHg. 2 (3.7%) patients had IOP of 30mmHg or more.
Out of the 54 cases with pseudoexfoliation, 29 (53.7%) were males and 25(46.3%) were females with male to female ratio of 1.16:1 while male to female ratio in non PEX patients was 0.907 (p value 0.380) as shown in table 2.
Table 2: Gender distribution.
|
Gender
|
Non PEX
|
PEX
|
Total
|
Chi-square value
|
p value
|
|
No. of cases
|
% age
|
No. of cases
|
% age
|
|
Male
|
450
|
47.6%
|
29
|
53.7%
|
479
|
0.770
|
0.380
|
|
Female
|
496
|
52.4%
|
25
|
46.3%
|
521
|
|
Total
|
946
|
100%
|
54
|
100%
|
1000
|
4 (7.4%) patients were of age 50 years or below, 6 (11.1%) patients were in the age group between 51-60 years. 27 (50%) patients were in the age group between 61-70 years. 11 (20.4%) patients were in the age group 71-80 years. 6 (11.1%) patients were in age above 80 as shown in table 3.
Table 3: Age distribution in PEX Patients.
|
Age group
|
No. of cases
|
Percentage
|
|
< 50
|
4
|
7.4%
|
|
51-60
|
6
|
11.1%
|
|
61-70
|
27
|
50.0%
|
|
71-80
|
11
|
20.4%
|
|
> 80
|
6
|
11.1%
|
|
Total
|
54
|
100.0%
|
Out of 54 PEX patient’s PXM on corneal endothelium was present in 5 (9.3%) patients. PXM was present on pupillary margin in 51 (94.4%) eyes (Figure 1), on iris in 31 (57.4%), iris transillumination defect was present only in 3 (5.6%). 25 eye (46.29%) had pseudo exfoliative material deposition on the iris, pupil, and anterior lens capsule simultaneously. Pseudoexfoliative material on anterior lens capsule (Figure 2) was present in 37 (68.50%), phacodonesis in 6 (11.1%), lens subluxation in 3 (5.6%) patients as shown in table 4.
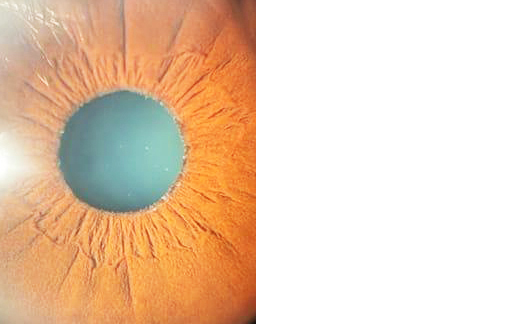
Figure 1: PEX on pupillary margin.
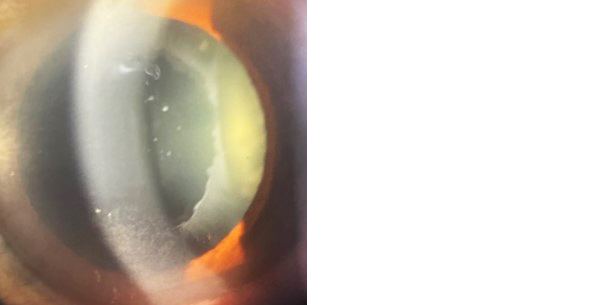
Figure 2: PEX on anterior lens capsule.
Table 4: Anterior segment findings in PEX patients.
|
Parameters
|
Number of patients
|
Percentage
|
|
PXM on cornea
|
5
|
9.3 %
|
|
PXM on pupillary margin
|
51
|
94.4%
|
|
PXM on iris
|
31
|
57.4%
|
|
ITD
|
3
|
5.6%
|
|
PXM on ALC
|
37
|
68.50%
|
|
Phacodonesis
|
6
|
11.1%
|
|
Lens subluxation
|
3
|
5.6%
|
Abbreviations: PEX: Pseudoexfolation, PXM: Pseudoexfoliative material, ITD: Iris transillumination defect, ALC: Anterior lens capsule.
Out of 54 patients with PEX, 12 (22.2%) patients had nuclear cataract, 3 (5.6%) patients had posterior subcapsular cataract, 11 (20.37%) patients had mature senile cataract, 6 (11.1%) patients had hyper mature cataract, 22 (40.7%) patients had mix form of cataract which includes nuclear+ PSC+ cortical cataract in 4 (7.42%) eyes, nuclear+ PSC in 8 (14.81%) and nuclear+ cortical cataract in 10 (18.52%) eyes as shown in table 5. Out of 54 PEX patients nuclear cataract was present in 34 (62.9%) patients. Nuclear sclerosis grade 2 was present in 7 (20.6%), nuclear sclerosis grade 3 in 13 (38.2%) and nuclear sclerosis grade 4 in 41.2% patients.
Table 5: Morphology of cataract in pseudoexfoliation patients.
|
Cataract
|
No. of patients
|
Percentage
|
|
Nuclear
|
12
|
22.20%
|
|
PSC
|
3
|
5.56%
|
|
MSC
|
11
|
20.37%
|
|
HMSC
|
6
|
11.11%
|
|
N+PSC+C
|
4
|
7.42%
|
|
N+PSC
|
8
|
14.82%
|
|
N+C
|
10
|
18.52%
|
|
Total patients
|
54
|
100.00%
|
Abbreviations: PSC: Posterior subcapsular cataract, MSC: Mature senile cataract, HMSC: Hyper mature senile cataract, N: Nuclear cataract, C: Cortical cataract.
On posterior segment evaluation, Fundus was normal in 26 (48.1%) of patients, Glaucomatous disc changes were present in 14 (25.9%) patients and in 14 (25.9%) patients fundus details were hazy due to dense cataract. On gonioscopy Pseudoexfoliative material (PXM) on trabecular meshwork was present in 24 (44.4%) eyes out of 54 patients and Sampaolesi’s line was present in 13 (24.1%) patients. out of 54 PEX patients, 30 (55.6%) had Shaffer’s grade 4 of anterior chamber angle, 16 (29.6%) had Shaffer’s grade 3, 6 (11.1%) patients had narrow angle (Shaffer’s grade 3) and 2 (3.7%) patients had extremely narrow angle (Shaffer’s grade 1) as shown in table 6.
Table 6: Gonioscopic evaluation of PEX patients.
|
Parameters
|
Number of patients
|
Percentage
|
|
PXM on TM
|
24
|
44.4%
|
|
Sampaolesi line
|
13
|
24.1%
|
|
Shaffer’s grading of angle of anterior chamber
|
|
Grade 4
|
30
|
55.6%
|
|
Grade 3
|
16
|
29.6%
|
|
Grade 2
|
6
|
11.1%
|
|
Grade 1
|
2
|
3.7%
|
Abbreviations: PXM: Pseudoexfoliative material
10(18.5%) patients had poor mydriasis (2-4 mm), 29(53.7%) of the patients had moderate mydriasis (>4-6 mm) and 15 (27.8%) patients had good mydriasis (>6mm) as shown in table 7.
Table 7: Dilated pupil size in PEX.
|
Pupil size
|
No. of cases
|
Percentage
|
|
>6mm
|
15
|
27.8%
|
|
>4- 6 mm
|
29
|
53.7%
|
|
2 - 4 mm
|
10
|
18.5%
|
|
Total
|
54
|
100.0%
|
Discussions
PEX is associated with multiple challenges during cataract surgery due to poor pupillary dilatation, zonular weakness. Extensive variations in prevalence of PEX have been reported ranging from 0 % in Eskimos to 38% in Navajo Indians. This variation in prevalence occurs because of cumulative effects of race, geographic location, ethnicity as well as sample size, study design, and diagnostic criteria.
The objective of the present study was to diagnose and evaluate the PEX syndrome from all patients admitted for cataract surgery in tertiary care centre of Uttarakhand. Out of 1000 screened patients 54 (5.4 %) patients were diagnosed of having pseudoexfoliation. In a retrospective study done by Bharadwaj et al in Eastern Uttar Pradesh PEX was reported in 3.8% patients [22]. The prevalence rate in south India was 3.8% in the study of Aravind et al in 2003 [14]. Most of the study subjects in our study were residents of remote, inaccessible hilly areas which may be one of the reasons for higher prevalence in our study.
PEX is common in the older population and rarely found below the age of 50 years. In the present study, mean age in PEX patients was found to be 67.48 + 9.79 years. The mean age of pseudoexfoliative syndrome patients in study conducted by Bharadwaj et al was 66.12±11.63 years, Arvind et al was 64.7±9.63 years, Triveni et al [23] was 68.47±9.37 years. In the present study 50% patients were in the age group between 61-70 years, 20.4% patients were in age group 71-80 years. In a study by Deepa et al the frequency of pseudoexfoliation was 36.53% in the age group of 61-70 years followed by 28.84% in the age group above 70 years, 23.07% in the age group between 51-60 years [6].
In present study out of the 54 cases with pseudoexfoliation, 29 (53.7%) were males and 25(46.3%) were females with male to female ratio of 1.16:1, with a slight male preponderance, with no statistically significant difference between the two groups (p value=0.38). In most of the studies, the predominance of males was more as compared to females. In the study conducted by Triveni et al [23], 66% patients were male. In a study by Joshi et al out of 226 pseudoexfoliation cases, 119 (52.7%) patients were males and 107 (47.3%) were females [18].
The present study shows a mean CCT of 528.46 + 18.49 microns in PEX patients in comparison to a mean CCT of 529.42+16.96 microns in non PEX patients with p value of 0.688 suggesting no significant difference between the two. This outcome is in accordance with some studies like those from Srinagar by Sajad et al in 2018 which the mean CCT in PEX patients was found to be 530 ± 25.45 microns, and from Turkey by Sirel et al where the average CCT in PEX patients was reported to be 548.0±28.55 microns in comparison to 547.29±33.80 microns in non PEX with the difference being statistically insignificant (p= 0.556) [24, 25]. The mean IOP was found to be 19.81±5.58 mm Hg which was significantly higher than non PEX patients (p value 0.001). Prior to cataract surgery, an IOP of more than 21 mm Hg was noted in 40.7% (n=54) of pseudoexfoliative eyes in comparison to 3.7% in non pseudoexfoliative eyes (n=946) and the difference was found to be statistically significant (p value= 0.001).
Pseudoexfoliative material on cornea in the present study was found in 5 (9.3%) of all PEX patients under study. It was seen that corneas with PEX had decreased average CCT as compared to other PEX eyes where cornea was without PEX. In a study by Triveni et al. 17.9% of PEX patients had corneal endothelial pigmentation, while a study by Sujani et al have reported 14% of PEX patients with corneal pigmentation [15]. In present study, PXM was present on pupillary margin in 51 (94.4%) eyes, PEX on iris was seen in 31 (57.4%). This is in concurrence with the study by Thomas in 2001 in which deposits of PEX on the iris sphincter and pupillary margin were seen in 84% of patients [26]. Triveni et al. in 2019 have reported 100% patients had PEX deposition on pupillary margin. Similar results are documented by Sujani et al stating, pupil margin is the most common site for pseudoexfoliative material deposition. In the present study, iris transillumination defect was noted in 3 (5.6%) of pseudoexfoliative eyes which concurs with study by Triveni et al [23] where iris transillumination defect was seen in 8.9% patients. PEX is associated with poor pupillary dilatation due to atrophy of the iris sphincter and iris stroma. Similar to results from previous literature, 72% of PEX patients had pupillary dilatation less than 6 mm. This is similar to the results of the study by Swetha et al wherein 96.7% eyes diagnosed with PEX syndrome had pupillary dilation of ≤6 mm [27]. Govetto et al have also reported that pupillary dilation is significantly less (p Value <0.001) in PEX patients than in non PEX patients [28]. The pseudoexfoliative material on the anterior lens capsule was found in 68% of pseudoexfoliative eyes (n=54) along with other ocular structures like iris, and pupil as noted in the present study.
Current study shows that 63% of pseudoexfoliative eyes had nuclear cataract, followed by mature cataract (20%) and hyper mature cataract (11%). The result of our study is comparable with Blue Mountain eye study where nuclear cataract was seen in 61.1% of eyes and Triveni et al. where nuclear cataract was present in 49% PEX patients [23, 29]. Nagrale et al in their study found 62% of PEX patient with nuclear cataract [30]. With the sclerosis of grade 4 being most common among nuclear cataract in present study, it is suggestive of delayed presentation of pseudoexfoliation syndrome patient to health centres. This could be attributed to issues related to awareness, transport, and a bit to the pandemic and measures taken to deal with it. In the present study, phacodonesis was found in 6 (11.1%), lens subluxation more than 180 degrees being visible in 3 (5.6%) patients and none of the patients had spontaneous lens dislocation. Triveni et al [23] have reported phacodonesis in 4.46 % eyes, while Sharma et al [19] reported phacodonesis in 8.23% eyes respectively.
In the current study PEX on trabecular meshwork was documented in 24 (44.4%) and Sampaolesi’s line was seen in 13 (24.1%) of pseudoexfoliative eyes. As per Shaffer’s grading, open angle (Grade 3, and Grade 4) was present in 85% patients, occludable (Grade 2) in 11% and closed angle (Grade1and less) in 2 (4%) patients. Results of our study are in accordance with study done by Philip et al. have shown open angles in 94.14% eyes of their patients and occludable angle in 1.86% eyes with pseudoexfoliation syndrome [27].
This data was collected in tertiary care centre in limited patients, multi-centre with more patients gives precise results. Tertiary centre data do not precisely reflect the disease profile of the community. Admittedly, the present study is based on a limited number of cases and is inadequate to provide conclusive data.
Conclusions
The prevalence of PEX was 5.4% in present hospital-based study in the Doon valley in patients aged 40 years and above, with more than 40% of such eyes recording an IOP more than 21mmHg, with high intraoperative complications should be considered a remarkable statistic. Therefore, dilated anterior segment evaluation should be emphasised in daily practices to avoid early PEX patients from being undiagnosed.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Lindberg JG. Clinical investigations on depigmentation of the pupillary border and translucency of the iris in cases of senile cataract and in normal eyes in elderly persons. Acta Ophthalmol Suppl. 1989; 190:1–96.
[2] Pranathi K, Magdum RM, Maheshgauri R. A study of complications during cataract surgery in patients with pseudoexfoliation syndrome. J Clin Ophthalmol Res. 2014; 2:7–11.
[3] Dvorak GT. Pseudo-exfoliation of the lens capsule: relation to ‘true’ exfoliation of the lens capsule as reported in the literature and role in the production of glaucoma capsulocuticulare. Am J Ophthalmol. 1954; 37:1–12.
[4] Thorleifsson G, Magnusson KP, Sulem P, Walters GB, Gudbjartsson DF, et al. Common sequence variants in the LOXL1 gene confer susceptibility to exfoliation glaucoma. Science. 2007; 317:1397–1400.
[5] Al-Saleh SA, Al-Dabbagh NM, Al-Shamrani SM, Khan NM, Arfin M, et al. Prevalence of ocular pseudoexfoliation syndrome and associated complications in Riyadh. Saudi Arabia. Saudi Med J. 2015; 36:108–112.
[6] Deepa R, Srinivasan G. Study of patients with pseudoexfoliation syndrome undergoing cataract surgery. Int J Ocul Oncol Oculoplasty. 2021; 7:184–189.
[7] Irkec M, Ustunel S, Orhan M, Ustunel S, Orhan M, et al. Systemic associations and prevalence of exfoliation syndrome in patients scheduled for cataract surgery. Eur J Ophthalmol. 2008; 18:551–555.
[8] Ritch R. Exfoliation syndrome-the most common identifiable cause of open-angle glaucoma. J Glaucoma. 1994; 3:176–177.
[9] Mitchell P, Wang JJ, Hourihan F. The relationship between glaucoma and pseudoexfoliation: the blue mountains eye study. Arch Ophthalmol. 1999; 117:1319–24.
[10] Ritch R, Schlotzer-Schrehardt U, Konstas AG. Why is glaucoma associated with exfoliation syndrome?. Progress Retinal Eye Res. 2003; 22:253–275.
[11] Konstas AGP, Ringvold A. Epidemiology of exfoliation syndrome. J Glaucoma. 2018; 27:4–11.
[12] Anastasopoulos E, Topouzis F, Wilson MR, Harris A, Pappas T, et al. Characteristics of pseudoexfoliation in the thessaloniki eye study. J Glaucoma. 2011; 20:160–166.
[13] Kim S, Lim SH, Sung KR, Yun SC, Kim CY, et al. Prevalence of pseudoexfoliation syndrome and associated factors in South Koreans: The Korean National Health and Nutrition Examination Survey. Ophthalmic Epidemiol. 2016; 23:298–302.
[14] Arvind H, Raju P, Paul PG, Baskaran M, Ramesh SV, et al. Pseudoexfoliation in South India. Br J Ophthalmol. 2003; 87:1321–1323.
[15] Sujani NB, Pravenya PK. Prevalence of ocular pseudo exfoliative syndrome in rural population: A study from South India. Indian J Clin Exp Ophthalmol. 2016; 2:231–237.
[16] Thomas R, Nirmalan PK, Krishnaiah S. Pseudoexfoliation in southern India: The Andhra Pradesh eye disease study. Invest Ophthalmol Vis Sci. 2005; 46:1170–1176.
[17] Krishnadas R, Nirmalan PK, Ramakrishnan R, Thulasiraj RD, Katz J, et al. Pseudoexfoliation in a rural population of Southern India: The Aravind Comprehensive Eye Survey. Am J Ophthalmol. 2003; 135:830–837.
[18] Joshi RS, Singanwad SV. Frequency and surgical difficulties associated with pseudoexfoliation syndrome among Indian rural population scheduled for cataract surgery: Hospital-based data. Indian J Ophthalmol. 2019; 67:221–226.
[19] Sharma PD, Kumar Y, Shasni RN. Pattern of pseudoexfoliation syndrome in lower to mid himalayan region of shimla hills in India. J Evol Med Dental Sci. 2013; 2:10098–10106.
[20] Parekh P, Green WR, Stark WJ. Electron microscopic investigation of the lens capsule and conjunctival tissues in individuals with clinically unilateral pseudoexfoliation syndrome. Ophthalmology. 2008; 115:614–619.
[21] Puska PM. Unilateral exfoliation syndrome: conversion to bilateral exfoliation and to glaucoma: a prospective 10-year follow-up study. J Glaucoma. 2002; 11:517–524.
[22] Bharadwaj R, Bhatt J, Sindhuja S. Clinical Characteristics of Pseudoexfoliation Syndrome and Pseudoexfoliation Glaucoma Patients. J Clin Diagn Res. 2022; 16:13–18.
[23] Triveni C, Divya N, Lakshmi G. A study of clinical spectrum of pseudoexfoliation syndrome. Trop J Ophthalmol Otolaryngol. 2019; 4:341–348.
[24] Sajad K, Snober Y, Asif J. Ocular profile of patients with Pseudoexfoliation syndrome and pseudoexfoliative glaucoma. J Med Sci Clin Res. 2018; 6:658–662.
[25] Sirel GG, Atilla B, Ahmet A, Aseana L. Clinical features of unilateral pseudoexfoliation syndrome. Turk J Ophthalmol. 2017; 47:5–8.
[26] Thomas H, Ursula SS, Gottfried HN. Unilateral or Asymmetric Pseudoexfoliation syndrome, An Ultra structural Study. Achieves Ophthalmol. 2001; 119:1023–1031.
[27] Swetha SP, Sheeja SJ, Arathi RS, Jasper S, Braganza AD. Clinical Profile in Pseudoexfoliation Syndrome in South India. Middle East African J Ophthalmol. 2012; 19:231–36.
[28] Govetto A, Lorente R, Parga PV, Rojas L, Moreno C, et al. Frequency of pseudoexfoliation among patients scheduled for cataract surgery. J Cataract Refract Surg. 2015; 41:1224–1231.
[29] Kanthan GL, Mitchell P, Burlutsky G, Rochtchina E, Wang JJ. Pseudoexfoliation syndrome and the long term incidence of cataract and cataract surgery: the Blue Mountain Eye Study. American J Ophthalmol. 2013; 155:83–88.
[30] Nagrale PH, Kesharaju V, Nandan N, Reddy K. A study of eyes with pseudoexfoliation, its association with cataract and its implications in cataract surgery. Int J Contemporary Med Res. 2018; 5:11–15.