Full Text
Introduction
Nasal obstruction is one of the most common complaints, with which a patient can present to otorhinolaryngologists in daily practice. Deviated nasal septum (DNS) is the most common cause of nasal obstruction. DNS can also cause impaired ventilation of paranasal sinuses leading to chronic sinusitis and snoring or sleep-related breathing disorders [1] when it is associated with hypertrophy of turbinates. Septoplasty is a common procedure that improves nasal breathing [2] and reduces sleep disturbances [1].
The evolution of nasal septum surgeries spans many years, marked by the development of increasingly advanced techniques. In the 18th century, Quelmaltz [3] recommended the application of daily digital pressure to correct septal deviations. Later, Adams⁴ introduced the use of steel screw compressors and daily splinting. Ingals [4] was the first to develop a technique for correcting septal deviation while preserving the bilateral mucosal flaps. In the 20th century, Gustav Killian [5] and Otto Tiger Freer [6] emphasized the importance of preserving the dorsal and caudal struts to maintain nasal support. It was Lanza and Stammberger [7, 8], who pioneered the technique of endoscopic septoplasty.
Thorough knowledge of the anatomy of the nasal septum and nasal valve with accurate preoperative diagnosis of pathologies of the septum in the context of the nasal cavity is essential for the success of surgery. Intraoperative visualization through an endoscope is very helpful for the surgeon and for training the residents. Different phases of the modern technique of endoscopic septoplasty are- approach, mobilization, resection/repositioning, and reconstruction/fixation.
Material and methods
A total number of 230 patients presented to the department of ENT, SVIMS-SPMCW a tertiary care referral center, Tirupati, Andhra Pradesh with clinical evidence of symptomatic DNS, an approach to endoscopic sinus surgeries and endonasal DCR (Dacryocystorhinostomy) were enrolled in this study from January 2018 to March 2022. The study was approved by the institutional ethics committee.
Patients with a history of trauma to the nose, atrophic rhinitis, benign tumors of the nose and paranasal sinuses or Sino nasal malignancies and invasive fungal sinusitis with septal involvement were excluded from the study.
Case files of all the patients included in the study were retrieved and information on clinical history, examination findings, investigations- DNE (Figure 1), CT PNS (Figure 2) (wherever done in indicated cases) as well as operative procedure and postoperative results and complications were extracted and reviewed.
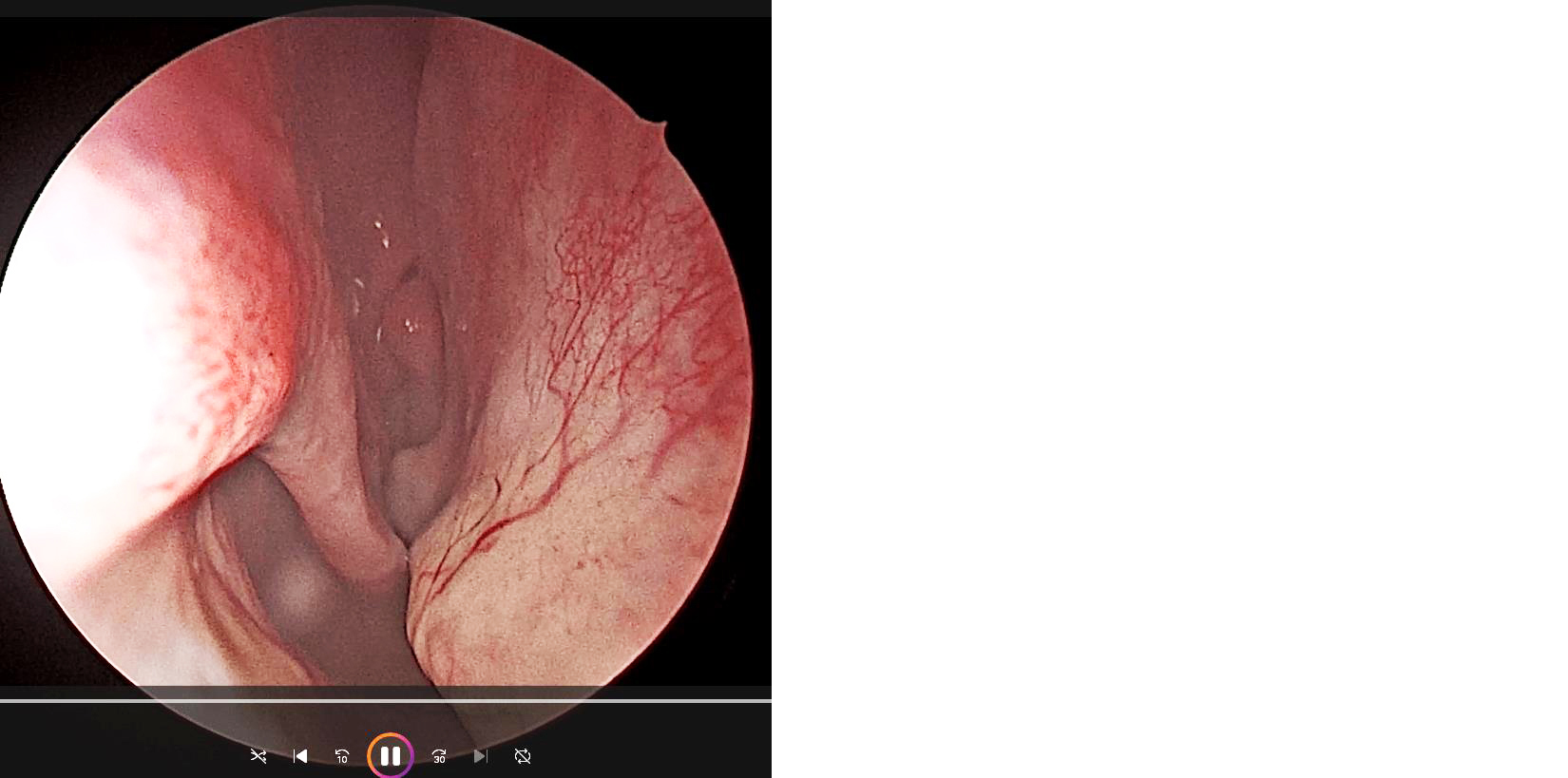
Figure 1: Endoscopic picture showing DNS with spur on right side.

Figure 2: CT PNS showing DNS with spur to right.
All these patients underwent endoscopic septoplasty by the same surgeon under general anesthesia after obtaining fitness from the anaesthesia team. After intubating with an appropriate-size endotracheal tube, the patient positioned supine with the head end elevated to 10 degrees and the head tilted slightly towards the surgeon. Bilateral nasal cavities decongested with 4% lignocaine with adrenaline and oxymetazoline solution. A preliminary nasal endoscopy was performed on all the patients with a zero-degree 4mm Hopkins endoscope. Both sides of the septum infiltrated with 1% lignocaine with 1 in 1,00,000 adrenaline. Freer’s incision was given on the left side (Figure 3a), mucoperichondrial and mucoperiosteal flaps elevated on the same side (Figure 3b). The bony cartilaginous junction was identified and dislocated. Opposite side mucoperiosteal flap elevated (Figure 3c). The deviated part of the bony and cartilaginous septum along with the spur removed(image 3d). Deviated maxillary crest if present- chiselled out. Flaps were repositioned and a diagnostic endoscopy was done again to assess the correction of septal deviation and also patency of nasal cavities. Flaps approximated and sutured with 3-0 chromic catgut (Figure 3e). Bilateral Nasal packing was done with an antibiotic-coated cuticel and treated with broadspectrum IV antibiotics, antihistamines, and analgesics. The patient was discharged on the second day after nasal pack removal.
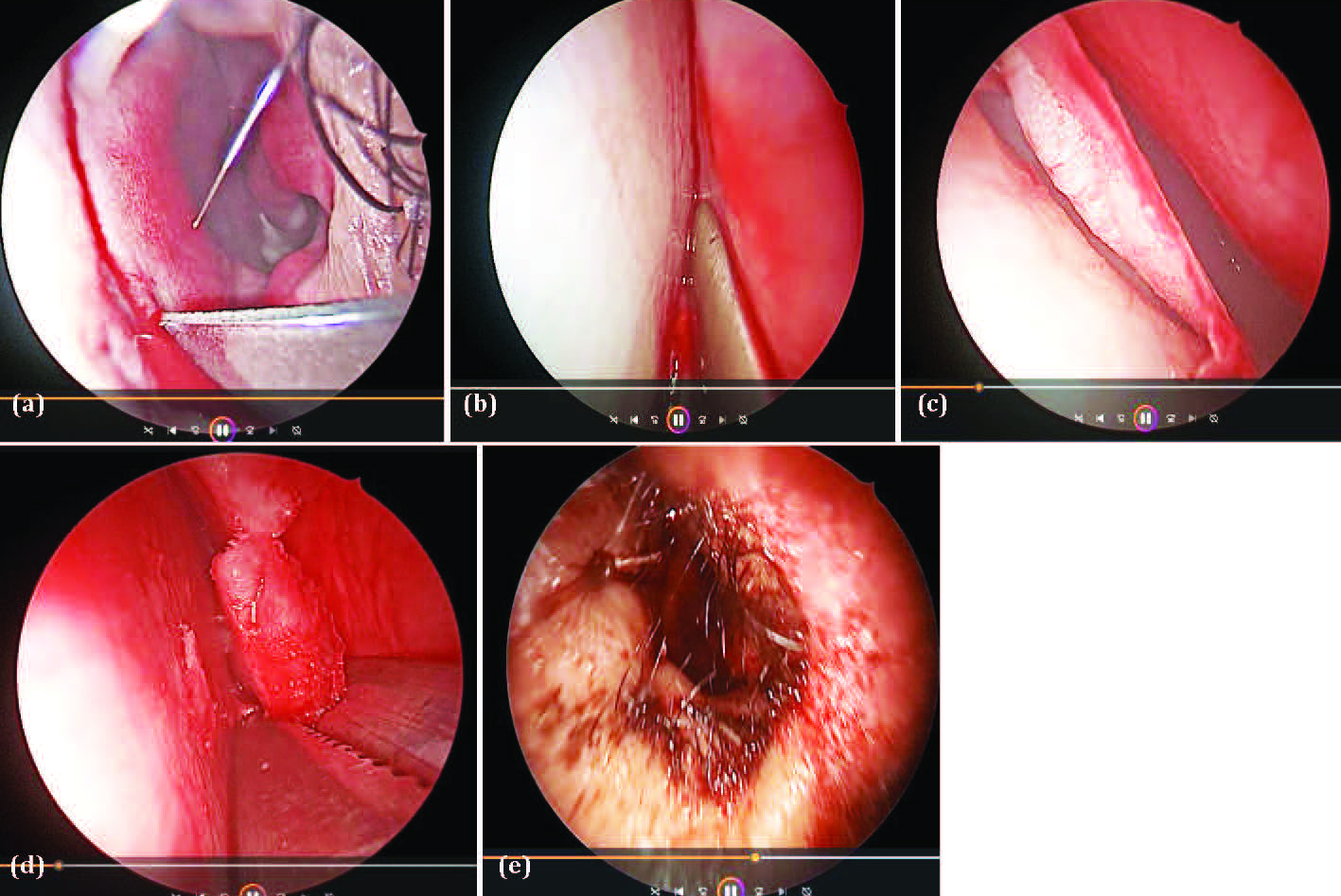
Figure 3: Images showing (a) Freer's incision, (b) mucoperichondrial flap elevation, (c) flap elevation on the opposite side, (d) removal of deviated bony septum, (e) sutured flaps.
All these patients were followed up for 6 months postoperatively -every week for the first 1 month, then every 15 days in 2nd month and then every month for the next 4 months. Nasal obstruction and symptom evaluation (NOSE) score was used to assess the postoperative symptomatic improvement during 1st, 3rd and 6th month followup as compared with the preoprative symptom score. NOSE score is a validated, disease specific subjective assessment questionnaire designed by Stewart et al in 2004 [9].
The extracted information was entered into MS Excel 2019 version and thereafter into Statistical Product and Service Solutions (SPSS) version 26.0 software.
Results
A total of 230 patients underwent the surgery during the study period. The age of the participants ranged between 17 and 67 years. There were 143 (62.1%) males and 87 (37.9%) females, and the age distribution ranged between 17 to 68 years with most of the patients falling in the range 21-30 years (Table 1) and the mean age of the patients who underwent septoplasty is 35.2+/- 13.3 years.
Table 1: Showing the distribution of gender and age distribution.
| |
Frequency
|
Percentage
|
|
Gender
|
| |
Males
|
143
|
62.1%
|
| |
Females
|
87
|
37.9%
|
|
Age groups
|
| |
<20 years
|
7
|
3.04%
|
| |
21-30 years
|
116
|
50.4%
|
| |
31-40 years
|
39
|
16.95%
|
| |
41-50 years
|
36
|
15.65%
|
| |
>51 years
|
32
|
13.9%
|
Most of the patients presented with nasal obstruction (67%), followed by nasal discharge (51%), postnasal drip (36%), headache (21%), snoring (10.4%) and watering of eyes, those having chronic Dacryocystitis (1.7%), epistaxis (1.3%). Few patients have more than one symptom (Table 2).
Table 2: Distribution of clinical features.
|
Clinical feature/Symptom
|
Frequency
|
Percentage
|
|
Nasal obstruction
|
154
|
67%
|
|
Anterior nasal discharge
|
117
|
51%
|
|
Postnasal drip
|
83
|
36%
|
|
Headache
|
48
|
21%
|
|
Epistaxis
|
3
|
1.3%
|
|
Snoring
|
24
|
10.4%
|
|
Watering of eyes
|
4
|
1.7%
|
Out of 230 patients who underwent endoscopic septoplasty during study period, 76(33%) patients underwent septoplasty alone as a primary procedure, 40 (17.4%) patients had inferior turbinate hypertrophy and so underwent septoplasty along with partial turbinectomy, 109 (47.4%) patients underwent FESS as a co-procedure along with septoplasty and 4 (1.7%) patients underwent septoplasty along with endoscopic endonasal DCR and one case is a revision septoplasty. Out of 47.4% of the patients, who underwent FESS along with septoplasty, 38% of the patients had sinonasal polyposis and 62% had chronic rhinosinusitis (Table 3).
Table 3: Surgical Procedures done with septoplasty.
|
Procedure
|
Frequency
|
Percentage
|
|
Septoplasty
|
76
|
33%
|
|
Septoplasty with partial turbinectomy
|
40
|
17.4%
|
|
Septoplasty with FESS
|
109
|
47.4%
|
|
|
DNS with CRS
|
67
|
62%
|
|
|
DNS with sinonasal polyposis
|
42
|
38%
|
|
Septoplasty with endo DCR
|
4
|
1.7%
|
|
Revision septoplasty
|
1
|
0.4%
|
In our study, complications like bleeding were seen in 1 patient (0.4%), septal perforation developed in 1 patient (0.4%), and synechiae developed in 1 patient (0.4%). Septal hematoma or abscess formation was not observed in any of these patients (Table 4).
Table 4: Showing the rate of complications.
|
Complication
|
No. of patients
|
Percentage
|
|
Septal perforation
|
1
|
0.4%
|
|
Bleeding
|
1
|
0.4%
|
|
Synichiae
|
1
|
0.4%
|
|
Septal hematoma
|
0
|
0
|
|
Septal abscess
|
0
|
0
|
In the present study, postoperative(1, 3, 6 month) improvement in different symptoms as compared to preoperative symptomatology- nasal obstruction, nasal stuffiness, mouth breathing, trouble sleeping, and troubled nasal breathing during exercise or on exertion are significant with p values < 0.000 for each symptom (Table 5). Values are the median (interquartile range) of symptom scores. P values are calculated using the Wilcoxon signed rank test based on positive ranks.
Table 5: Showing comparison of symptom score preop and postoperatively.
|
Symptom
|
preop
|
Postop 1 month
|
Postop 3 and 6 months
|
P values
|
|
Preop vs postop 1month
|
Preop vs postop 3 and 6months
|
|
Nasal obstruction
|
4(1-4)
|
2(1-3)
|
0(0-1)
|
0.000*
|
0.000*
|
|
Nasal stuffiness
|
4(1-4)
|
2(1-3)
|
0(0-1)
|
0.000*
|
0.000*
|
|
Mouth breathing
|
3(1-4)
|
1(1-2)
|
1(0-1)
|
0.000*
|
0.000*
|
|
Trouble sleeping
|
3(1-4)
|
1(1-2)
|
0(0-1)
|
0.000*
|
0.000*
|
|
Trouble breathing during exercise
|
4(1-4)
|
1(1-2)
|
1(0-1)
|
0.000*
|
0.000*
|
*Significant.
Discussion
In this study, male predominance (62%) was noted, which is similar to that of Al-Shehri AM et al study which reported 60% male preponderance [10], Nawaiseh et al found 70% male preponderance [11] and Ngamdu et al reported 78.6% of male preponderance in their study [12].
In our study, the most common presenting symptom is nasal obstruction (67%), followed by nasal discharge (51%), postnasal drip(36%), headache (21%), snoring (10.4%), watering of eyes (1.7%) and epistaxis (1.3%). Nasal obstruction is the preponderant complaint in our study which corresponds to the studies of Al-Shehri et al study [10], Nawaiseh et al study [11] and Ngamdu et al study [12], which shows 55%, 91.6% and 100% respectively.
In the present study septoplasty with FESS(47.4%) is the most commonly done procedure followed by septoplasty (33%), septoplasty with partial turbinectomy (17.4%), septoplasty with endoscopic endonasal DCR (1.7%) and revision septoplasty (0.4%) which was corresponding to that of Chung et al study [13] who reported that concomitant procedures performed with endoscopic septoplasty included endoscopic sinus surgery (81.9%), turbinate reduction (44.8%), and rhinoplasty (4.3%). Vandenbroeck [14] reported ESS (81.9%) and turbinate reduction (13.1%) as the accompanying surgeries. On the other hand our study is antonymous to the study of Kulkarni [15] where septoplasty (62.6%) alone was done as a primary procedure followed by FESS with septoplasty in (9.2 %), septo-rhinoplasty (9.9 %) cases and DCR with septoplasty (18.3 %).
According to Brennan et al [16] the ideal objective of septal surgery is a permanent correction of deviation without any complications. Complication rate in our study is about 1.2% which includes bleeding (0.4%), septal perforations (0.4%), and synechiae (0.4%). overall complication rate in other studies like Nawaiseh et al [11], Kulkarni [15] and Bhennur et al [17] are 3.2%, 1.2% and 2.67% respectively.
In the present study there was a significant improvement in the symptomatology of all patients at postop 1st,3rd, and 6th-month follow-ups as compared to pre-op symptomatology which is similar to the studies of Kulkarni et al [15], Bugten et al [18].
Endoscopic septoplasty provides an improved field of vision, especially critical areas of the nose like the nasal valve area and posterior deviations, chances of flap tear are less. Serves as a valuable teaching tool when used in conjunction with video monitors as compared to the traditional headlight technique.
In the modern era, because of the ease of availability of equipment, endoscopic septoplasty does not have any major drawbacks except for difficulty in correcting caudal dislocations another drawback is the duration of the surgery is comparatively longer as compared with conventional technique.
Conclusion
Endoscopic septoplasty is a minimally invasive surgery that can be performed either alone or as a concurrent procedure along with other nasal surgeries with good postoperative outcomes.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Ertugay CK, Toros SZ, Karaca CT, Yilmaz HB, Kilic K, et al. Is septoplasty effective on habitual snoring in patients with nasal obstruction? Eur Arch Otorhinolaryngol. 2015; 272:1687–1691.
[2] Karlsson TR, Shakeel M, Supriya M, Ram B, Ah-See KW. Septoplasty with concomitant inferior turbinate reduction reduces the need for revision procedure. Rhinology. 2015; 53:59–65.
[3] Meloni F, Bozzo C, De Peacock MR. Sub-mucous resection of the nasal septum. J Laryngol Otol. 1981; 95:341–356.
[4] Subramaniam V, Basheer M, Hosagadde RS. Evolution of correction of the deviated nasal septum—a historical overview. Arch Med Health Sci. 2018; 6:293–297.
[5] Killian G. Die submucose fensterresektion der nasenscheidewand. Arch Laryngol Rhinol. 1904; 16:362–387.
[6] Freer OT. The correction of nasal septum with a minimum of traumatism. JAMA. 1902; 38:636–642.
[7] Lanza DC, Kennedy DW, Zinreich SJ. Nasal endoscopic and its surgical application. In: Lee KJ, editor. Essential Otolaryngology: Head and Neck Surgery. New York: Medical Examination Publishing Co. 1991; p.373–387.
[8] Stammberger H. Functional endoscopic sinus surgery: the Messerklinger technique. Philadelphia: BC Decker. 1991; p.432–433.
[9] Ghosh SK, Dutta M, Haldar D. Role of bilateral inferior turbinoplasty as an adjunct to septoplasty in improving nasal obstruction and subjective performance in patients with deviated nasal septum associated with allergic rhinitis: an interventional, prospective study. Ear Nose Throat J. 2023; 102:445–452.
[10] Al-Shehri AM, Amin HM, Necklawy A. Retrospective study of endoscopic nasal septoplasty. Biomed Res. 2013; 24:337–340.
[11] Nawaiseh S, Al-Khtoum N. Endoscopic septoplasty: retrospective analysis of 60 cases. J Pak Med Assoc. 2010; 60:796–798.
[12] Ngamdu YB, Kirfi AM, Adamu A, Abubakar A, Edem KP, et al. Endoscopic septoplasty: a retrospective analysis of indications and outcome. J West Afr Coll Surg. 2023; 13:78–81.
[13] Chung BJ, Batra PS, Citardi MJ, Lanza DC. Endoscopic septoplasty: revisitation of the technique, indications, and outcomes. Am J Rhinol. 2007; 21:307–311.
[14] Vandenbroeck S, Jorissen M. Endoscopic septoplasty: literature review, surgical techniques and retrospective analysis at the University Hospitals Leuven. J Laryngol Otol. 2019; 133:262–268.
[15] Kulkarni SV, Kulkarni VP, Burse K, Bharath M, Bharadwaj C, et al. Endoscopic septoplasty: a retrospective analysis of 415 cases. Indian J Otolaryngol Head Neck Surg. 2015; 67:248–254.
[16] Hwang PH, McLaughlin RB, Lanza DC, Kennedy DW. Endoscopic septoplasty: indications, technique and results. Otolaryngol Head Neck Surg. 1999; 120:678–682.
[17] Bhennur DP, Polisetti RB, Lanke S, Krishna Sasanka KSB. Endoscopic septoplasty—our experience. J Evid Based Med Healthc. 2015; 2:8631–8633.
[18] Bugten V, Nilsen AH, Thorstensen WM, Moxness MHS, Amundsen MF, et al. Quality of life and symptoms before and after nasal septoplasty compared with healthy individuals. BMC Ear Nose Throat Disord. 2016; 16:13.