Full Text
Introduction
Chondrosarcoma is a malignant cartilaginous tumor of mesenchymal origin. It is very rare and accounts for 8% of all head and neck sarcomas and 0.1% of all head and neck malignancies [1]. It is seen anywhere in the body, the most common sites being pelvis, ribs and long bones. Cs of nose and paranasal sinuses is extremely rare. In the nasal cavity, most common site is nasal septum [2]. Highest incidence seen in 4-5 decade of life and males are slight more commonly affected than females [3]. Usually it presents with the symptoms of nasal obstruction and epistaxis [4],very rarely presents with ocular symptoms like proptosis and visual distrubances [5]. Intracranial extension also seen in some cases.
Here we are reporting a case of 26-years-old male patient who has been diagnosed with a mass in the nose and paranasal sinuses with orbital and intra cranial extension.
Case report
A 26-years-old male patient presented to our department with complaints of proptosis of left eye with watering since 2 months (Figure 1a). No history of visual disturbances. Patient also had a history of similar complaints two years ago. For that he underwent craniofacial resection of mass in the left nasal cavity in some other hospital. Biopsy of the mass revealed as enchondroma. He presented to our department with recurrence of symptoms. We did diagnostic nasal endoscopy (DNE). It revealed a mass is in the bilateral nasal cavities with perforation of posterior part of septum (Figure 1b).

Figure 1a: Proptosis of left eye.

Figure 1b: DNE showing a mass in the nasal cavity.
He was advised CECT of orbits and para nasal sinuses. It showed a large non enhancing soft tissue mass within the posterior nasal cavity causing erosion of nasal septum, cribriform plate and crista galli. The mass seen extending into left maxillary sinus with erosion of medial wall of left maxillary sinus. And also it is extending into left orbit by erosion of left lamina papyracea.
MRI brain, paranasal sinuses and orbits of both plain and contrast showed a 48*37*41.6 mm sized lobulated lesion appearing heterogeneously hyper intense on T2/FLAIR and hypo intense on T1 weighted image with few calcific foci in the nasal cavity. The lesion is seen abutting and displacing left medial rectus muscle and left globe laterally, superiorly it is abutting the dura of frontal lobe with erosion of cribriform plate, crista galli (Figure 2a & 2c) and obliteration of left maxillary ostium with maxillary sinusitis (Figure2b).The lesion causing erosion of nasal septum, bony trabeculae of ethmoid sinus, medial walls of bilateral orbits (Lt>Rt) and also abutting bilateral middle and inferior turbinates.
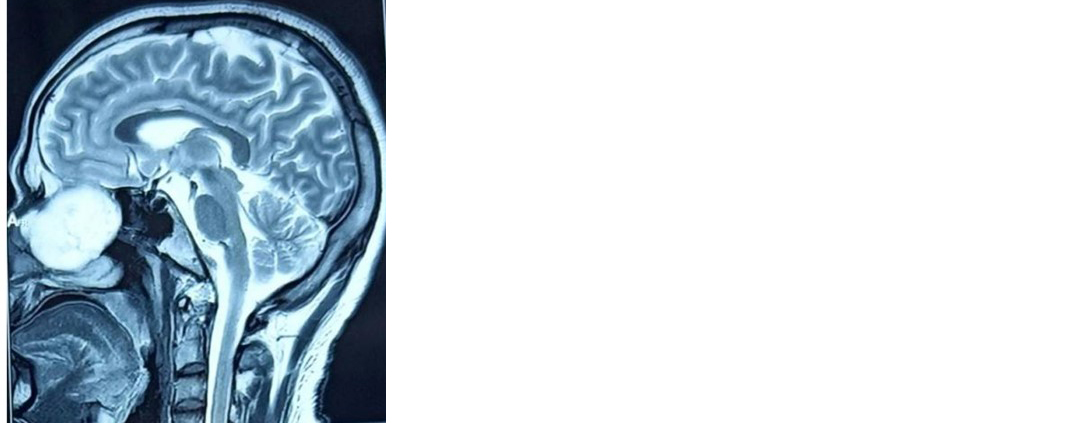
Figure 2a: T2 weighted MRI sagittal section showing the lesion extending into dura of the frontal lobe.
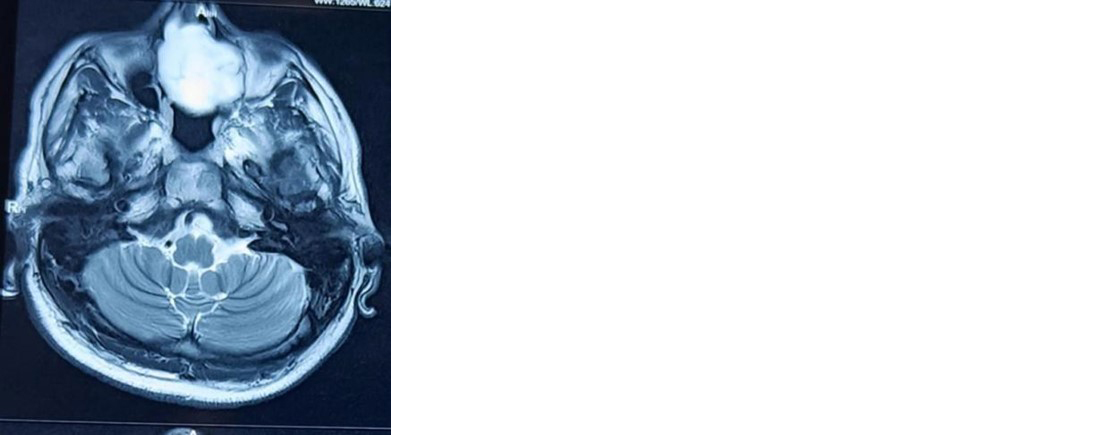
Figure 2b: T2 weighted MRI Axial section showing a mass in the nasal cavity with erosion of medial wall of left orbit.

Figure 2c:T2 weighted MRI coronal section showing a lesion causing erosion of cribriform plate, crista galli and extending into dura of the frontal lobe with erosion of medial wall of bilateral orbits.
Patient was taken up for the surgery. Bifronto-orbito-craniotomy was done by bicoronal incision. Bone flap elevated and gross total tumor excision was done (Figure 3a). Frontal sinus packed with fat. Bone flap fixed with plates and screws. Nasal part of the tumor was excised endoscopically (Figure 3b). Nasal packing was done with merocel. Haemostasis was achieved.

Figure 3a: Intra operative image showing excision of mass by craniotomy approach.

Figure 3b: Intra operative picture of endoscopic excision of tumor.
Tissue sent for Histopathological (HPE) examination. It showed irregular shaped lobules of cartilage varying in size and shape. These lobules are separated by fibrous bands. Chondrocytes are typically varying in size and shape containing enlarged heterochromatic nuclei (Figure 4a,b) with focal calcifications. All these features are suggestive of well differentiated grade 1 chondrosarcoma.
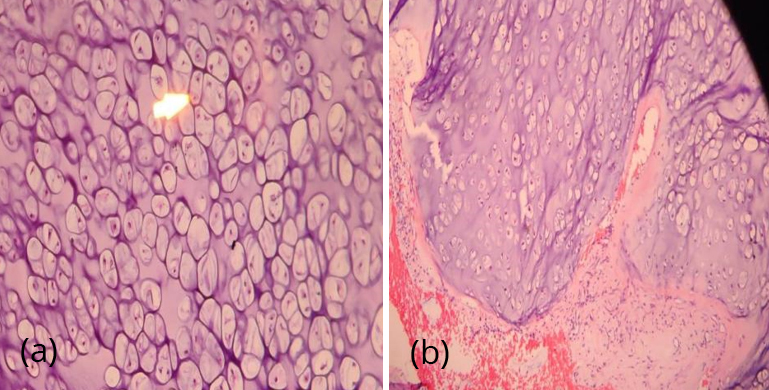
Figure 4a,b: Microscopic examination with H&E staining showing lobules of cartilage separated by fibrous bands. Chondrocytes with hyper chromatic nuclei.
After surgery patient was sent for radiotherapy. Pre RT MRI was done 3 weeks after the surgery, it showed 2.9*1.1.cms lesion in frontal sinus, with extension into adjacent ethmoidal air cells, left orbit, left maxillary and sphenoid sinuses (figure 5a,b).
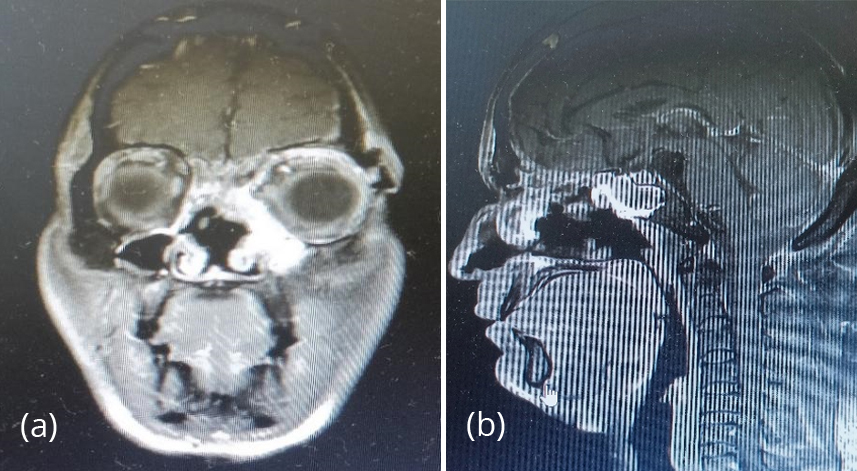
Figure 5: (a) Pre RT MRI brain coronal cuts showing heterogeneously hyper intense lesion in left frontal sinus with extension into ethmoids and left maxillary sinus. (b) Pre RT MRI brain sagittal section showing a lesion in sphenoid sinus.
Patient received 66 Gy radiation in 30 fractions to gross residual tumor, 60 Gy in 30 fractions to pre-operative bed and 54 Gy in 30 fractions to entire sphenoid sinus, left maxillary sinus and medial wall of right orbit, delivered by image guided radiation therapy (IGRT).
After 3 months of radiotherapy patient came for follow up. MRI brain was repeated. It showed a decrease in the tumor volume with persistent residual tumor. The lesion was heterogeneously enhancing in the right side of the nasal septum (Figure 6a), extending into adjacent ethmoidal air cells, left maxillary sinus and left orbit (Figure 6b).
As the patient is symptomatically better, does not have any complaints, he was advised to follow up after 6 months (Figure 7).
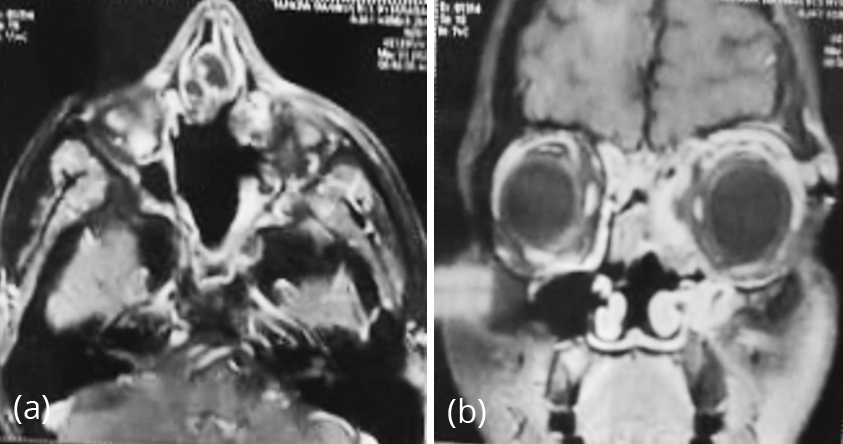
Figure 6: (a) MRI brain axial cut showing heterogeneously hyper intense lesion in right side nasal cavity with pushing the septum to opposite site. (b) .MRI brain coronal cut showing lesion extending into adjacent ethmoids, left maxillary sinus and left orbit.

Figure 7: Post-operative picture after 3 months of surgery showing improvement in the proptosis.
After 6 months of follow up, DNE was done. It showed a mucosal thickening near the septum on right side and all sinuses were appear clear (Figure 8a, b).

Figure 8: (a) DNE showing mucosal thickening near the septum on right side, (b) DNE showing all sinuses are appear clear.
Discussion
Chondrosarcoma is a malignant cartilaginous tumor of mesenchymal origin. It is very rare and accounts for only 4% of non-epithelial tumors of nose and para nasal sinuses [1]. It is seen anywhere in the body, the most common sites are being pelvis, ribs and long bones. CS of nose and paranasal sinuses is extremely rare. In the nasal cavity, most common site is nasal septum [2]. It is usually seen in 4th-5th decades of life. Males are most commonly affected than females [3].
Symptoms depends on site of involvement by the tumor. It is presented with common nasal symptoms like nasal obstruction and epistaxis [4]. Ocular symptoms are proptosis and visual distrubances [5]. Aetiology of CS is not clearly understood, but it may be due to trauma, previous surgery, irradiation, fibrous dysplasia and due to exposed to beryllium [6].
Early diagnosis is difficult, because it mimics like other common sino nasal conditions. Histopathologically differentiating low grade chondrosarcoma from chondroma is very difficult [7].
CT and MRI are important imaging modalities for diagnosis, preoperative planning and to evaluate the tumor characteristics. The common diagnostic findings in CT scan are destruction and calcification of lesions which erodes the surrounding bones [8].
Histopathological examination used for confirmation of diagnosis. Based on the histology, CS are divided into three type, Grade 1 well differentiated, Grade 2 moderately differentiated and Grade 3 poorly differentiated. This grading helps in prognosis and clinical behaviour of the tumor [9].
As the tumor is radio resistant, surgical excision is the treatment of choice [10]. The type of surgery depends upon extension of the tumor, histological grade and location of the tumor [11]. Adjuvant radiotherapy is indicated for residual and recurrent lesions. Due to its tendency for recurrence and progressive spread, it has poor prognosis [12].
Conclusion
Whenever the patient presents with the common and non-specific symptoms with mass in the nasal cavity, a possibility of chondrosarcoma should be considered in the diagnosis along with the common diagnostic considerations. Radiological investigations like CT and MRI plays an important role in the diagnosis. Multidisciplinary approach is needed to treat this kind of tumors. Long term follow up is needed for proper outcome.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Malika EO, Ben Njima M, Mouna B, Zeineb N, Wassim K, et al. Chondrosarcoma of the nasal cavity and paranasal sinuses: a rare entity. Ear Nose Throat. 2024; 24:01455613241249028.
[2] Eide JG, Kshirsagar RS, Harris JC, Civantos A, Brody RM, et al. Multi‐institutional review of sinonasal and skull base chondrosarcoma: 20‐year experience. Head Neck. 2022; 44:2686–2695.
[3] Berhili S, Guerrouaz MA, Oulhouq Y, Terrab FZ, Moukhlissi M, et al. Sino-nasal low-grade chondrosarcoma revealed by isolated bilateral loss of sight: an unprecedented presentation of a rare tumour. Radiol Case Report. 2022; 17:2563–2657.
[4] Bouhafs K, Lachkar A, Bouamama T, Miry A, Benfadil D, et al. Nasosinusal chondrosarcoma with orbito-cerebral extension. J Surg Case Rep. 2022; 2022:rjac286.
[5] Nguyen MT, Farahvash A, Dickson BC, Lee JM, Cusimano MD, et al. Sinonasal chondrosarcoma presenting with isolated severe vision loss. J Neuro-Ophthalmol. 2021; 41:e752–e755.
[6] Sahu PK, Goyal L, Bothra J, Shashivadhanan, Sharma P. Chondrosarcoma of nasal cavity: a rare entity. Indian J Sur Oncol. 2020; 11:288–292.
[7] Swain SK, Samal S, Sahu MC. Chondrosarcoma at the sinonasal region. BLDE Univer J Health Sci. 2019; 4:30–33.
[8] Sachdeva K, Sachdeva N. Myxoid chondrosarcoma of nasomaxilloethmoid region with intracranial extension. Indian J Otolaryngol Head Neck Surg. 2016; 68:110–114.
[9] Magnano M, Boffano P, Machetta G, Garibaldi E, Delmastro E, et al. Chondrosarcoma of the nasal septum. Eur Arch Oto-Rhino-Laryngol. 2015; 272:765–772.
[10] Belgioia L, Vaccara EM, Bacigalupo A, Corvò R. Management of nasal septum chondrosarcoma occurring in elderly: a case report. Cureus. 2017; 9:e1497.
[11] Guo L, Liu J, Sun X, Wang D. Sinonasal tract chondrosarcoma: 18-year experience at a single institution. Auris Nasus Larynx. 2014; 41:290–293.
[12] Coca-Pelaz A, Rodrigo JP, Triantafyllou A, Hunt JL, Fernández-Miranda JC, et al. Chondrosarcomas of the head and neck. Eur Arch Oto-Rhino-Laryngol. 2014; 271:2601–2609.