Full Text
Introduction
Breast cancer is one of the most common malignancies found in women across the world [1]. The majority of them almost 50% requiring surgery which ranges from breast‑conserving technique to radical mastectomy. Severe acute postoperative pain following surgery not only increases the risk of persistent pain and restricted shoulder mobility, it also leads to longer hospitalization and increased healthcare costs [2]. Effective analgesia in patients greatly modifies the pathophysiological response to stress, prevents or reduces postoperative complications and improves patient recovery.
PECs (pectoralis nerve block) is a interfacial plane block, which includes PECs type I and PECs type II block which are ultrasound guided approaches for the blocking of the pectoral nerves, long thoracic nerves and intercostal nerves from 3rd to 6th intercostal space. This was developed by Blanco et al in 2011 [3].
Ultrasound guided PECs blocks do not result in sympathetic blocking, hypotension, pneumothorax, or spinal cord injuries, in contrast to paravertebral, epidural, and thoracic paravertebral blocks [4]. Along with these benefits, they also lessen the need for intraoperative narcotics and reduce post-operative nausea and vomiting. They also increase patient comfort and shortens hospital stay.
The primary objective of the study was to evaluate and compare the postoperative analgesic efficacy in patients undergoing modified radical mastectomy under general anaesthesia with and without pectoralis nerve block.
Materials and methods
After obtaining institutional ethical committee approval, this prospective randomised study was conducted at HIMS teaching hospital, Hassan. Fifty adult female patients of the American Society of Anaesthesiologists (ASA) status I and II, between 30 and 65 years, scheduled to undergo elective unilateral modified radical mastectomy for carcinoma breast were assessed for eligibility and enrolled into the study after written informed consent.
Patients with a history of coagulopathy, psychological disorders, neurological disorders, significant cardiac disorders, local infections, or refusals to consent for participation were excluded from the study.
All enrolled patients were taught and explained to report their postoperative pain intensity on a visual analogue scale (VAS) of 0–10 cm where 0 meant no pain and 10 stood for worst possible pain. All patients on arrival to operation theatre were secured with 18G cannula and ringer lactate started at 10ml/kg. Standard monitoring like non-invasive blood pressure, electrocardiography and pulse-oximetry were connected and basal vitals noted. Pre-medication done with Inj midazolam 0.05mg/kg.
Patients belonging to Group A received ultrasound guided PECs (I & II) block. The patient was kept supine with the ipsilateral upper limb in abducted position, the skin over the ipsilateral breast and adjoining infraclavicular and axillary regions was disinfected with betadine and sterile draping of the area was done. A linear USG probe of high frequency (6–13 MHz) of a portable ultrasound system (SonoSite, Micromaxx Bothell, Washington, USA) was taken; the probe was covered with a sterile dressing and a sterile conductivity gel was applied.
The USG screen's imaging depth was adjusted to 4-6 cm. The axillary vessels directly above the first rib were located by moving the USG probe laterally after it was initially positioned cephalo-caudally in the infraclavicular area. Further lateral and downward probe movements allowed for the identification of the third and fourth ribs. The probe was then moved as needed and suitable anatomical structures were found, such as the serratus anterior muscle and the pectoralis major and minor muscles.
A skin puncture site aligned with the probe was chosen and 2 milliliters of 1% lignocaine were infiltrated, with the image centered at the level of the third rib. A 21G 100 mm short bevelled insulated needle (Stimuplex A, B Braun, Melsungen AG, Germany) was used for the block, and it was inserted into the fascial plane between the serratus anterior and pectoralis minor muscles using a medial-to-lateral in-plane approach. After aspiration in real time, a volume of 20 ml of ropivacaine 0.5% was injected in increments of 5 ml. After that, 10 ml of 0.5% ropivacaine was injected into the fascial plane between the pectoralis major and minor muscles. The pin-prick test was used to assess sensory block.
Both Group A and Group B participants recieved Inj fentanyl 2 μg/kg and induced with Inj propofol 2 mg/kg titrated to loss of verbal response. Vecuronium 0.12 mg/kg used to facilitate tracheal intubation with ET tube of size 7.5mm.
Anaesthesia maintained with nitrous oxide and oxygen (70% plus 30%) and isoflurane (0.8%–1%) MAC with maintenance doses of IV vecuronium 0.02 mg/kg. Inj. Fentanyl 0.25 μg/kg IV was given for any increase in HR and systolic blood pressure (SBP) more than 20% from pre‑induction value.
Towards the completion of surgery, isoflurane discontinued neuromuscular blockade was reversed by IV neostigmine 0.05 mg/kg with glycopyrrolate 0.01 mg/kg and extubated. Postoperative pain scores was assessed using a visual analogue scale and whenever the VAS > 4, Inj Tramadol 1.5mg/kg was given.
The primary outcome measures were postoperative analgesia duration (time to first rescue analgesia), secondary outcome measures included total post‑operative analgesic requirement (tramadol consumption) in the first 24 h, haemodynamic changes and any adverse effects such as post‑operative nausea and vomiting (PONV), local anaesthetic (LA) toxicity and pruritus postoperatively. All patients were followed up in surgical wards post operatively, all data were observed, recorded, tabulated and statistically evaluated.
Sample size was calculated using Statistical Package for Social Sciences [SPSS] for Windows Version 22.0 Released 2013. Armonk, NY: IBM Corp, based on the literature from the previous study done by Kumar et al, for the mean difference in the time for first rescue analgesia [1]. The significance level was set at 0.05, the power of the study was 0.80. After calculation the sample size in each group was 25 patients.
Results
Total of 60 patients were screened for eligibility and 50 patients were recruited into the study who met all the inclusion criteria. These fifty patients were randomised into two groups such that both groups were comparable in terms of demographic profile i.e. age and ASA grading which are shown in table 1 and shows no statistically significant difference (Figure 1).
Table 1: In this table during post-operative period time to requirement of first rescue analgesia (Inj Tramadol) has been compared among both Group A and Group B, the time duration in minutes. *p <0.05 when compared with Group A and Group B.
|
Post-op analgesia
|
Group A
|
Group B
|
p value
|
|
Mean
|
SD
|
Mean
|
SD
|
|
Post-op analgesia (in min)
|
832.8
|
102.94
|
134.6
|
37.66
|
<0.001
|
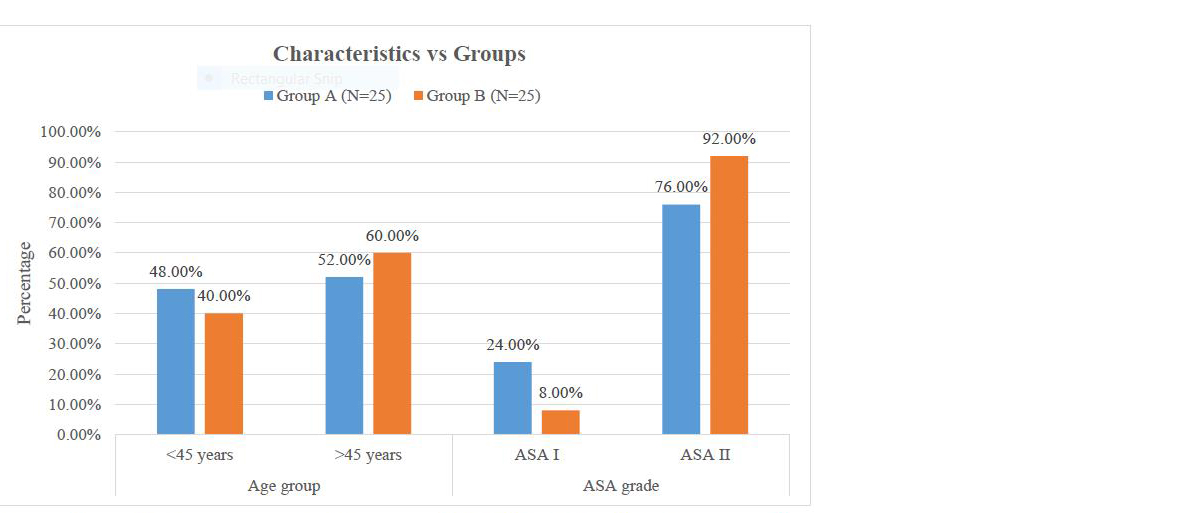
Figure 1: In this figure comparison of demographic data has been done, it shows the division of age group as less than 45 and more than 45 years, also it shows comparison of American Society of Anaesthesiologist (ASA) grading of the patients.
Regarding mean duration of post-operative analgesia among both the groups, which was measured in terms of time to first rescue analgesia. The time duration in Group A 832.80 ± 102.94 minutes (i.e. 13.87 ±1.71 hrs) was significantly higher than Group B 60 ± 37.66 minutes (i.e. 2.24 ±0.6 hrs) (Figure 2).
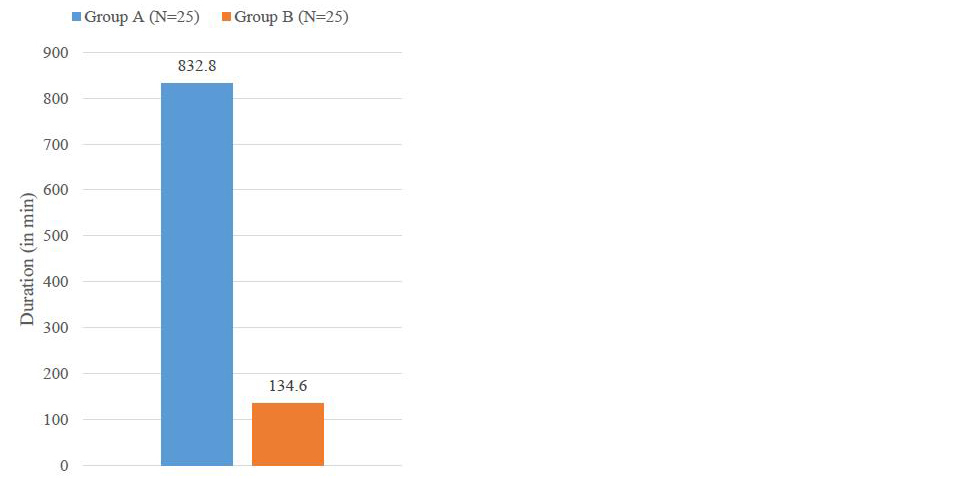
Figure 2: Total mean duration of post operative analgesia after the procedure among two groups i.e. the Group A which has received the USG PECs block and the Group B with only general anesthesia. *p<0.05 compared with group A and group B.
Further when the total requirement of tramadol in both the groups was compared in Group it A was 140.00 ± 54.96 mg which was significantly lesser than Group B which was 370.80 ± 49.98 mg (Table 2) (Figure 3). We compared the haemodynamic variables (HR, SBP, DBP and MAP) in both the groups at all the time intervals measured intraoperatively and the change in heart rate, blood pressure was statistically insignificant at all intervals (Figure 4 and 5).
Table 2: In this table total Tramadol consumption as rescue analgesic in the post operative period has been compared between Group A and Group B. *p < 0.05 when compared between Group A and Group B.
|
Tramadol consumption
|
Group A
|
Group B
|
p value
|
|
Mean
|
SD
|
Mean
|
SD
|
|
Total tramadol consumption (in mg)
|
140
|
54.96
|
370.8
|
48.98
|
<0.001
|
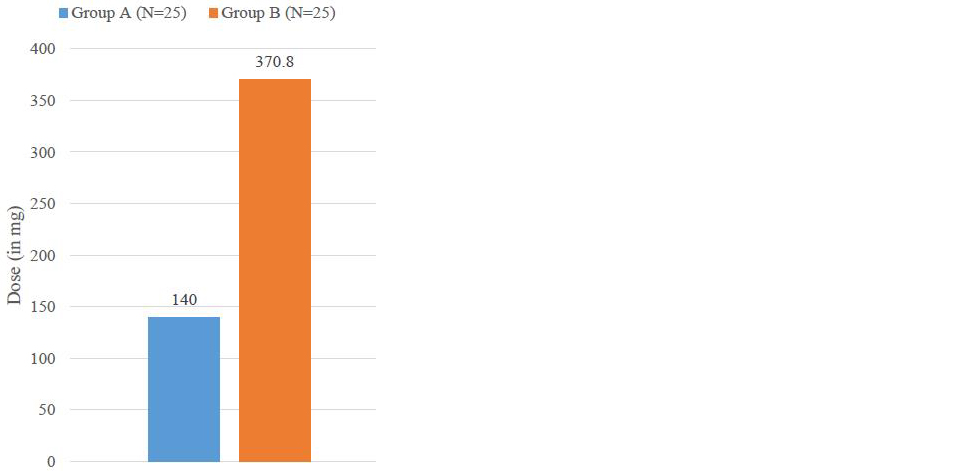
Figure 3: In post-operative period, the total requirement of Inj Tramadol to manage pain has been compared among both the groups in this figure. *p<0.05 compared with Group A and Group B.
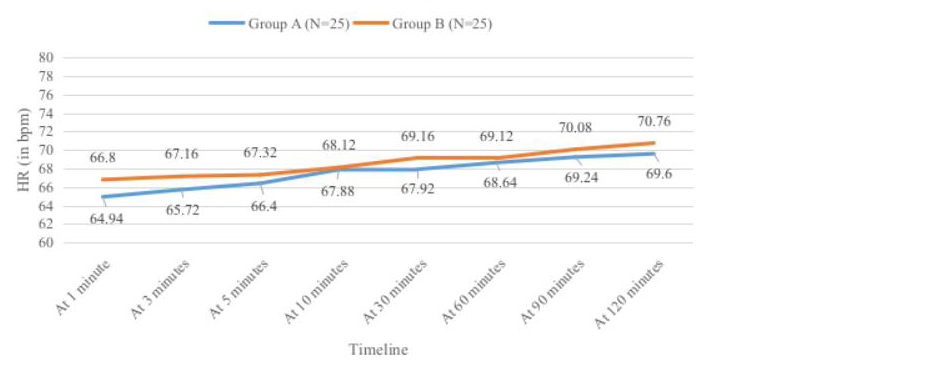
Figure 4: Heart rate at different time interval, Group A has lesser values than Group in intra-operative period.*P<0.05 compared with Group A and Group B.
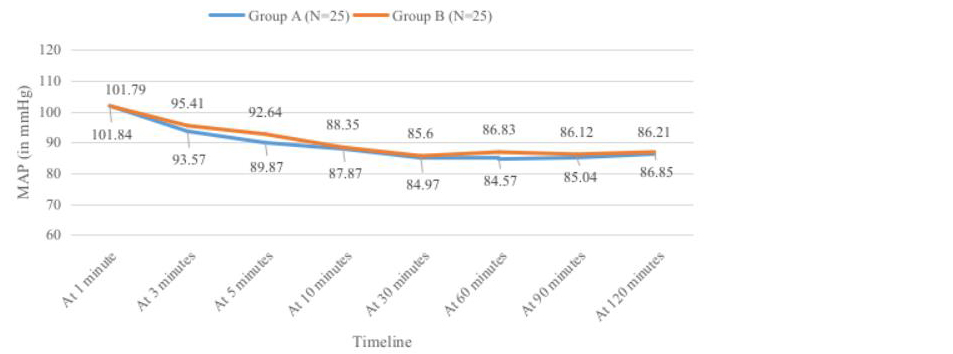
Figure 5: Mean arterial pressure at different time interval, Group A has lesser values than Group in intra-operative period.*p<0.05 compared with Group A and Group B.
Discussion
The incidence of breast carcinoma has increased in recent years and their treatment involves radical surgery which is associated with severe pain post-operatively and use of opioids results in side effects like sedation, confusion, nausea, vomiting, ileus, hypotension, and respiratory depression [1, 6]. In this study we supplemented general anaesthesia with PECS block in order to reduce the opioid requirement post-operatively and thereby minimising the side effects of them. Blanco and colleagues first used this block in 2011 using levo-bupivacaine 0.25% among 50 patients and found that PECs block helps to reduce opioid requirement post-operatively [3].
In PECs I and II the nerves blocked are the intercostobrachial and lateral cutaneous branches of the intercostal nerves (T2–T6), the medial cutaneous nerve of the arm and forearm, and the long thoracic and thoracodorsal nerves [3].
Effective post-operative analgesia not only helps in faster recovery, it also helps in preventing chronic pain since it blocks the pectoral nerves, which are not only motor nerves it also transports proprioceptive and nociceptive fibres. Hence the combined use of this will result in an excellent analgesia [7].
In our study on 60 patients undergoing modified radical mastectomy (MRM) we compared the post-operative analgesia among Group A which received PECs block along with general anesthesia and Group B which received only general anesthesia to find out Group A had better post-operative analgesia i.e. 832.80 ± 102.94 minutes (i.e. 13.87 ±1.71 hrs) when compared to Group B which had mean duration of 134.60 ± 37.66 minutes (i.e. 2.24 ±0.6 hrs).
Similarly when tramadol consumption in first 24hrs was compared, in Group A it was significantly less (140±54 mg) when compared to Group B (370.80±48.98 mg). These study findings were consistent with a similar study done by Kumar et al [1]. In another study Cylwik et al evaluated the efficacy of PECs block and their results were similar to our study [5].
Ahmed et al conducted a study comparing paravertebral block and PECs block among 30 patients undergoing MRM and concluded that PECs block provides better pain relief than paravertebral block [6]. Deng et al in their study on PECS II block compared ropivacaine in different concentrations and observed that 0.4% ropivaicaine had better results. In this study 0.5 % ropivacaine was used and the results were consistent with their study [9].
Zhao et al in their meta-analysis concluded that PECs block helped to reduce both intra-operative as well as post-operative consumption of opioids thereby lesser side effects [10]. When intra-operative haemodynamic parameters were compared like the heart rate, mean arterial pressure the values were statistically insignificant. Adverse effects like local anesthesia toxicity, nausea, vomiting and pruritis were not seen in this study.
Use of ultrasound avoided the risk of pleural puncture, it provided real time images and helped in accurate delivery of the drug in the interfacial plane thereby providing maximum blockade. Bakshi et al have reported difficulty during surgery due to fluid filled spaces after PECs block which was not encountered in our study [11].
Our study limitations include no shams block was given to Group B subjects as it was considered ethically incorrect, the chronic pain after the surgery was not followed-up in our surgeries and also patients were not blinded. However further studies are required with larger sample size for a precise data and opioid free anesthesia could be administered for patients requiring modified radical mastectomy.
Conclusion
To conclude PECs block definitely helped to reduce the post-operative opioid consumption thereby reducing the side effects of opioids, which helped in better recovery of the patients.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Kumar S, Goel D, Sharma SK, Ahmad S, Dwivedi P, et al. A randomised controlled study of the postoperative analgesic efficacy of ultrasound-guided pectoral nerve block in the first 24 h after modified radical mastectomy. Indian J Anaesth 2018; 62:436–442.
[2] Neethu M, Pandey RK, Sharma A, Darlong V, Punj J, et al. Pectoral nerve blocks to improve analgesia after breast cancer surgery: A prospective, randomized and controlled trial. J Clin Anesth. 2018; 45:12–17.
[3] Blanco R. The 'pecs block': a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011; 66:847–848.
[4] Sinha C, Kumar A, Kumar A, Prasad C, Singh PK, et al. Pectoral nerve versus erector spinae block for breast surgeries: A randomised controlled trial. Indian J Anaesth. 2019; 63:617–622.
[5] Cylwik J, Celińska-Spodar M, Bud, N. Evaluation of the efficacy of pectoral nerve-2 block (PECS 2) in breast cancer surgery. J Pers Med. 2023; 13:1430.
[6] Ahmed MAM, Elhenawy AME, Awad HGS. Comparative study between intraoperative and postoperative analgesic effect of ultrasound-guided thoracic paravertebral block versus pectoral nerve block in patients undergoing modified radical mastectomy: a randomized controlled trial. Ain-Shams J Anesthesiol. 2022; 14:13.
[7] Ataollahi MR, Sharifi J, Paknahad MR, Paknahad A. Breast cancer and associated factors: a review. J Med Life. 2015; 8:6–11.
[9] Deng W, Fu D, He L. Evaluation of pectoral nerve block in modified radical mastectomy: comparison of three concentrations of ropivacaine. Clin Interv Aging. 2020; 15:937–944.
[10] Zhao J, Han F, Yang Y, Li H, Li Z. Pectoral nerve block in anesthesia for modified radical mastectomy: A meta-analysis based on randomized controlled trials. Medicine (Balti more). 2019; 98:e15423.
[11] Bakshi SG, Shetmahajan M, Thota RS. Pectoralis block for breast surgeries: More than postoperative analgesic. Indian J Anaesth. 2019; 63:243–245.