Orginal Research
2025
March
Volume : 13
Issue : 1
A comparative study on the efficacy and safety of the distal transradial access and conventional transradial access in primary percutaneous coronary intervention
Santhosh KS, Ravi M, Unni TG, Benjamin B, Cenchery PK
Pdf Page Numbers :- 59-65
Santhosh KS1, Manoj Ravi1,*, Govindan Unni T1, Bino Benjamin1 and Prasanna Kumar Cenchery1
1Department of Cardiology, Jubilee Mission Medical College & Research Institute, Thrissur, Kerala, India, 680005
*Corresponding author: Dr. Manoj Ravi, Associate Professor, Department of Cardiology, Jubilee Mission Medical College & Research Institute, Thrissur, India. Email: drmanojravicardio@gmail.com.
Received 7 October 2024; Revised 25 November 2024; Accepted 3 December 2024; Published 11 December 2024
Citation: Santhosh KS, Ravi M, Unni TG, Benjamin B, Cenchery PK. A comparative study on the efficacy and safety of the distal transradial access and conventional transradial access in primary percutaneous coronary intervention. J Med Sci Res. 2025; 13(1):59-65. DOI: http://dx.doi.org/10.17727/JMSR.2024/13-11
Copyright: © 2025 Santhosh KS et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Distal transradial access (dTRA) in anatomical snuff box has advantages over the conventional transradial access at wrist (wTRA). There is limited data of dTRA in primary Percutaneous Coronary Intervention (PCI). The objective was to study the efficacy and safety of dTRA as compared to wTRA in primary percutaneous coronary intervention.
Methods: 100 patients undergoing primary PCI were randomly allocated into dTRA and wTRA groups with 50 each in a group. The procedural characteristics and complications were comparatively analyzed.
Results: Access success in dTRA group was 86% vs 100% in wTRA (p-0.012). Access crossover from dTRA to wTRA was 14%. Overall higher puncture attempts were needed in dTRA group (p<0.001). First attempt success in dTRA was 46% vs 80% in wTRA (p<0.001). Median puncture attempts in both groups was ‘one’. Mean puncture time (73.56±55.52 sec vs 30.06±16.79 sec, p<0.001) and mean access time (94.95±60.02 sec vs 45.7±17.96 sec, p<0.001) were higher in dTRA group. 6F introducer sheaths used in all cases in both groups. In both the groups mean total procedure time, fluoroscopy time and dose area product (DAP) were similar. Lower incidence of hematoma was noted in dTRA group (4.7% vs 14%) (p-0.169).
Conclusion: dTRA offers to be a promising alternative with better ergonomics and lower vascular complications in Acute Coronary Syndromes (ACS). Access time has a learning curve effect, which can ease with experience.
Keywords: anatomical snuff box; conventional transradial access; distal transradial access; primary percutaneous; coronary intervention
Full Text
Introduction
Science has evolved over the years, so are its methods and techniques. Vascular access for percutaneous coronary intervention (PCI) evolved from brachial to transfemoral, and then to transradial access (TRA). TRA is superior to transfemoral access with lower bleeding and vascular complications. Also, there is a reduction in mortality and acute kidney injury in acute coronary syndrome (ACS) with TRA [1]. Hence currently conventional TRA at wrist (wTRA) is the choice of access in primary PCI. However, apart from the shortcoming of keeping an arm in supination with extended wrist, which is not comfortable for the patient, the most important complication of wTRA is radial artery occlusion (RAO). RAO seen in about 4%, restricts the use of the radial artery (RA) for dialysis fistula or coronary artery bypass grafting (CABG) in future [2]. Also, if left side access is indicated, the wTRA poses ergonomic challenges to the operator.
The distal tarnsradial access (dTRA) at the anatomical snuff box (ASB) for coronary catheterization was introduced in 2017 by Dr F Kiemeneij [3]. ASB is a triangular depression over the dorsum of the hand, bounded medially by extensor pollicis longus and laterally by extensor pollicis brevis. Advantages of dTRA are based on the anatomic and physiologic rationale [4]. Distal RA arises after several anastomotic branches. Even its occlusion, won’t compromise flow to hand hence, reducing occurrence of RAO. Absence of major venous structures with the floor formed by carpel bones, it has a better compression hemostasis. Its superficial course above facial compartments of hand, avoids compartment syndrome. With the patients left arm positioned close to groin, operator need not bend over. The patient does not have restriction of dominant right hand, thus dTRA has better ergonomics both to patient and operator [3, 5]. It’s a better choice for operators who prefer left approach to coronaries. These advantages would be more beneficial to patients undergoing primary PCI as they are at high risk of bleeding and access site complications given higher use of anticoagulants, antiplatelets like P2Y12 inhibitors and glycoprotein IIb/IIIa inhibitors. However, there is a paucity of data regarding the dTRA in primary PCI.
The objective was to study the efficacy and safety of dTRA as compared to wTRA in primary percutaneous coronary intervention.
Methods
This observational study was conducted at Department of Cardiology, Jubilee Mission Medical College & Research Institute, Thrissur from April 2021 to November 2022 after obtaining approval from institutional ethical committee. The study included 100 patients presenting with ACS, undergoing primary PCI and having a palpable radial pulse at the ASB. Post CABG and patients having AV fistula were excluded. To avoid the effect of experience on endpoint, the procedure was performed by a single operator. Before starting the study, technical feasibility of obtaining dTRA was checked in 25 cases, and the study was initiated after achieving 80% success rate without any complication. Patients were allocated into two groups (50 in each) the dTRA and wTRA groups randomly. Demographic and clinical variables were collected. Patients were followed during and post PCI. The endpoints of procedural characteristics and complications were compared among the groups.
dTRA technique
The presence of an appropriate radial pulse in the ASB was verified by palpation. The left forearm was positioned on the groin while applying ulnar deviation and semiflexion of wrist with semipronation of the forearm. After local anesthesia the artery was punctured with a 21G needle at an angle of 35-45 degrees. Through the puncture needle a guide wire is inserted. Over the guidewire a radial hydrophilic sheath is introduced. To prevent arterial spasm nitroglycerine (100mcg) and unfractionated heparin (5000 IU) was given through the sheath. Through this radial sheath the PCI was performed. Post PCI sheath removed, and elastic compressor bandage was applied. (Figures 1-5). All patients were evaluated at 4 - 6 hours. On removal of compressor bandage the presence of a palpable distal radial pulse and hematomas were noted. In the absence of a palpable radial pulse, distal RAO was considered present.

Figure 1: Presence of an appropriate distal radial pulse in the ASB verified by palpation. Roll of gauze grasped to favor a shift of the distal radial artery to the surface of the radial fossa.

Figure 2: The left forearm was positioned on the groin while applying ulnar deviation and semi-flexion position at the wrist and semipronation of the forearm.
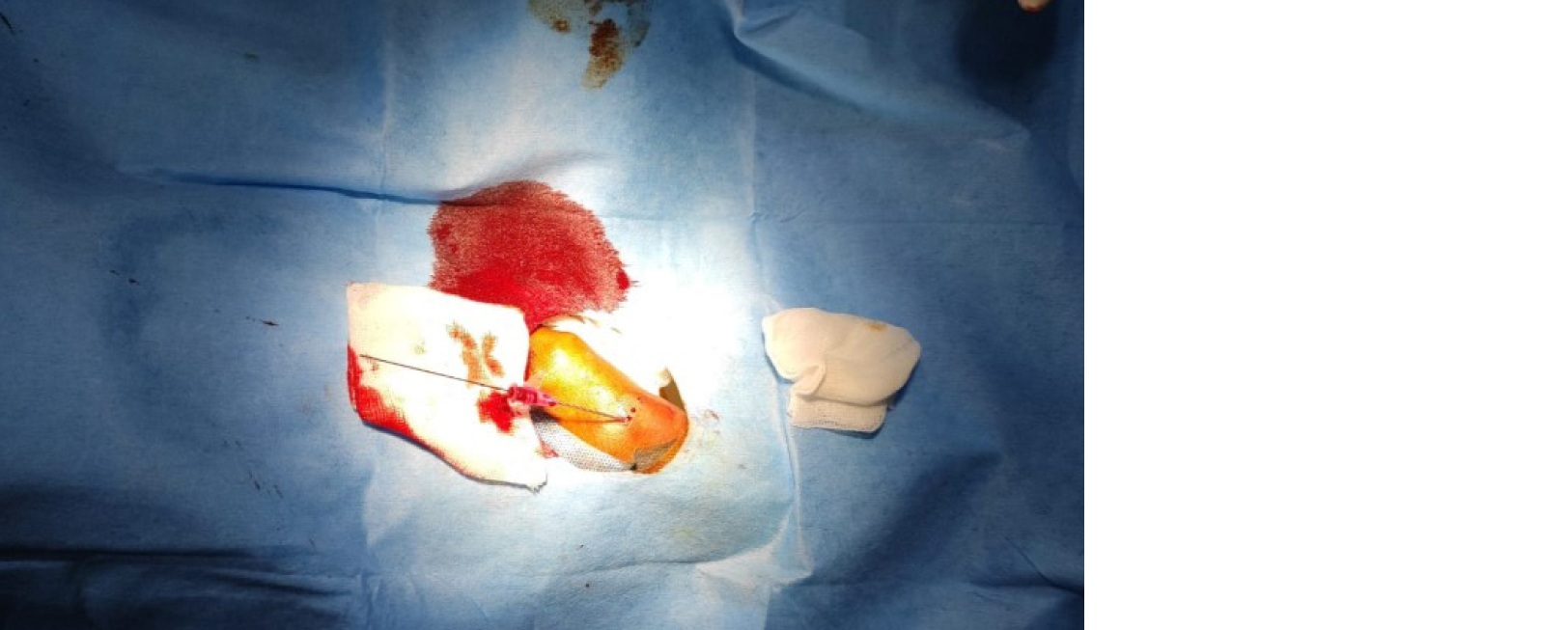
Figure 3: Puncture cannula with guide wire inserted.
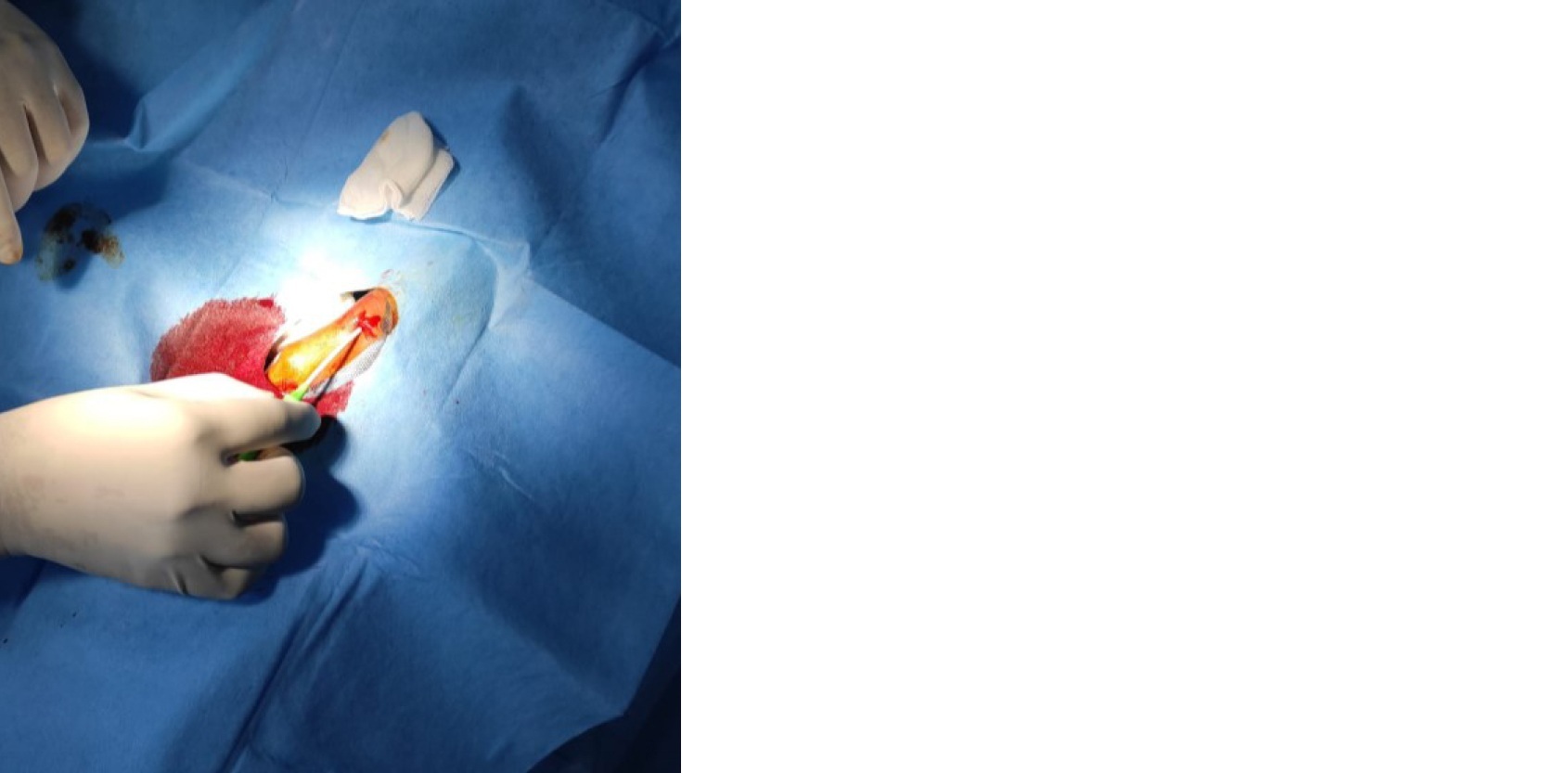
Figure 4: Introducer sheath being inserted.
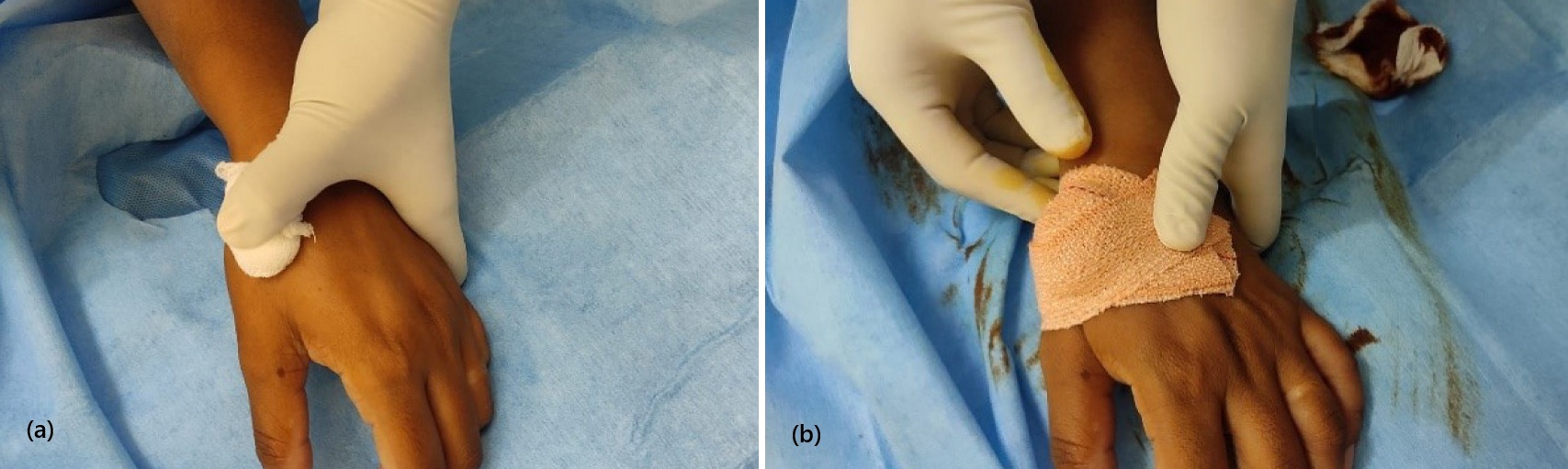
Figure 5a, b: Application of compression bandage.
Endpoints and definitions
The composite primary endpoints of procedural efficiency in terms of procedural characteristics was achievement of puncture success (guidewire introduction), puncture time (time from puncture needle contact to passing of guidewire), puncture attempt (each insertion of the needle in the skin), access time (time between anesthesia needle contact to insertion of introducer sheath) , access success (when an introducer sheath is placed through the artery), total procedure time (time between needle prick for local anesthesia and final disengagement of catheter), and access switch (when puncture is unsuccessful and switched to other access). Safety endpoints were puncture site complications, including hematoma, and radiation exposure in each case measured as total fluoroscopic time (FT), and the dose area product (DAP).
Statistical analysis
Descriptive and inferential statistical analysis done. The student t test (two tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups (Inter group analysis) on metric parameters. Leven`s test for homogeneity of variance has been performed to assess the homogeneity of variance. Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups, non-parametric setting for qualitative data analysis. The Statistical software namely SPSS 22.0, and R environment ver.3.2.2 were used.
Results
Table 1 summarizes the clinical characteristics among the two groups, dTRA and wTRA. Of the 50 patients in each group, the age distribution was comparable. Over all 44% in the study belonged to >60 years of age. Mean age in both groups were 58 years. In both the dTRA and wTRA groups majority were males i.e 84% and 68% respectively. T2DM was present in 58% of dTRA and 46% in wTRA grous (p = 0.317). In dTRA and wTRA groups 38% and 44% respectively were hypertensive (p = 0.680). 36% in both groups were smokers (p-0.846). Mean systolic BP in the dTRA and wTRA groups were 124mmHg and 114mmHg respectively (p = 0.053). Mean diastolic BP were 82mmHg and 71.1 mmHg in the dTRA and wTRA groups respectively (p<0.002).
Table 1: Baseline clinical characteristics of the study population.
|
Variables
|
GROUP dTRA
|
GROUP wTRA
|
Total
|
P Value
|
|
Age (Years)
|
58.94±12.59
|
58.2±11.81
|
58.57±12.15
|
0.762
|
|
Gender
|
|
|
Female
|
8(16%)
|
16(32%)
|
24(24%)
|
0.100
|
|
|
Male
|
42(84%)
|
34(68%)
|
76(76%)
|
|
T2DM
|
29(58%)
|
23(46%)
|
52(52%)
|
0.317
|
|
HTN
|
19(38%)
|
22(44%)
|
41(41%)
|
0.680
|
|
DLP
|
21(42%)
|
24(48%)
|
45(45%)
|
0.689
|
|
CKD
|
2(4%)
|
3(6%)
|
5(5%)
|
1.000
|
|
Smoking
|
18(36%)
|
18(36%)
|
36(36%)
|
0.841
|
|
Diagnosis
|
|
|
AWMI
|
24(48.0%)
|
24(48.0%)
|
48(48.0%)
|
1.000
|
|
|
IWMI
|
26(52.0%)
|
26(52.0%)
|
52(52.0%)
|
|
BP
|
|
|
Systolic BP(mmHg)
|
124.98±28.14
|
114.88±23.26
|
119.93±26.18
|
0.053
|
|
|
Diastolic BP(mmHg)
|
82.52±18.35
|
71.1±17.54
|
76.81±18.76
|
0.002
|
|
HB (g/dl)
|
14.83±2.11
|
14.26±2.16
|
14.55±2.14
|
0.188
|
|
PCV (%)
|
43.41±6.98
|
42.7±5.96
|
43.06±6.46
|
0.585
|
|
TC (cells/µl)
|
11118.6±2990.5
|
12735.4±4751.59
|
11927±4032.53
|
0.044
|
|
Blood Urea (mg/dl)
|
26.54±9.38
|
24.72±9.5
|
25.63±9.44
|
0.338
|
|
Serum Creatinine (mg/dl)
|
1.06±0.32
|
0.96±0.31
|
1.01±0.32
|
0.104
|
|
RBS(mg/dl)
|
205.3±105.23
|
188.74±85.24
|
197.02±95.64
|
0.389
|
|
INR
|
0.98±0.17
|
0.98±0.12
|
0.98±0.15
|
0.884
|
|
Total cholesterol (mg/dl)
|
231.52±56.55
|
224.1±47.27
|
227.81±51.98
|
0.478
|
|
Triglycerides (mg/dl)
|
216.94±194.7
|
175.72±84.3
|
196.33±150.7
|
0.173
|
|
LDL (mg/dl)
|
150.08±42.05
|
147.1±36.51
|
148.59±39.21
|
0.706
|
|
HDL (mg/dl)
|
43.32±14.46
|
43.58±10.3
|
43.45±12.49
|
0.918
|
|
Culprit Vessel
|
|
|
LAD
|
20(40.0%)
|
26(52%)
|
46(46.0%)
|
0.005
|
|
|
LCX
|
7(14%)
|
5(10%)
|
12(12%)
|
|
|
RAMUS
|
1(2%)
|
0(0%)
|
1(1%)
|
|
|
RCA
|
15(30%)
|
19(38%)
|
34(34%)
|
Abbreviations: HB- Hemoglobin, PCV- Packed cell volume, TC- Total counts, LAD- left anterior descending artery, LCX- left circumflex artery, RCA- Right coronary artery.
Table 2 summarizes the procedural characteristics and complications among the two study groups. Puncture was successful in 43 (86%) in the dTRA group compared to 100% in the wTRA group (p = 0.012). In 7(14%) of the dTRA group puncture was unsuccessful as compared to none in wTRA group. These 7 included 2 females who were switched to wTRA. Among the puncture successful patients, majority, i.e 46% in dTRA and 80% in wTRA had successful puncture in 1 attempt. Median puncture attempt was 1 in both the groups. Puncture time among the majority i.e 38% of dTRA was between 30-60 seconds, as compared to wTRA where 52% had puncture time of <30 seconds and 42% had between 30-60 seconds (p<0.001). Mean puncture time was 1 minute 14 seconds in dTRA group as opposed to 30 seconds in the wTRA group (p<0.001). All patients who had successful punctures had successful access in both the groups. 6F introducer sheath was used in all successful cases in both the groups. None had radial spasm in either group. Among the patients who had successful access, access time in the dTRA was > 1minute in 56% and between 30seconds to 1 minute in 28%. However, the majority, i.e 39(78%) in wTRA had access time of 30 seconds to 1 minute (p = 0.118) (Figure 6).
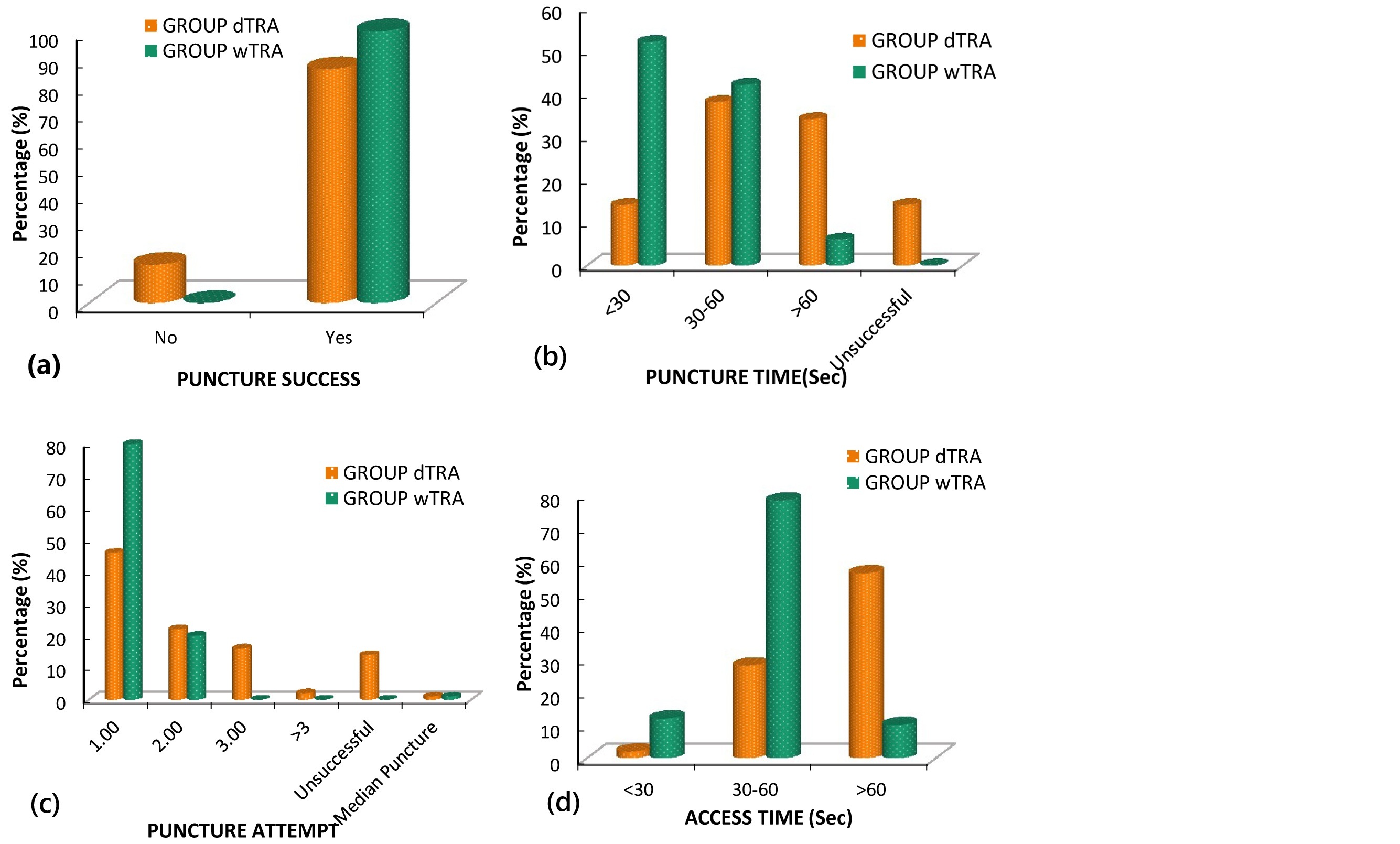
Figure 6a-d: Graphs of procedural characteristics of the two groups.
Mean puncture time was 73.56±55.52 sec in dTRA compared to 30.06±16.79 seconds in wTRA (p<0.001). In dTRA group the access time was 94.95±60.02 seconds as opposed to 45.7±17.96 seconds in the wTRA group (p<0.001). Mean overall puncture time and access time was 50.17±45.09 seconds and 68.47±49.26 seconds respectively. Mean total procedure time in dTRA and wTRA groups were 45.72±14.81 mins and 43.24±14.46 mins respectively (p=0.417). Majority in both the groups i.e 81% and 78% had a total procedure time of more than 30 minutes. Mean fluroscopy time in both the dTRA and wTRA groups are comparable i.e 616 seconds and 592 seconds respectively (p=0.603). Mean DAP among the dTRA and wTRA groups are 89.6 Gycm2 and 83.1 Gycm2 respectively (p=0.616). Hematoma was the only complication noted among both the groups. It was seen in 2 (4.7%) of dTRA and 7(14%) of wTRA groups (p=0.169).
Table 2: Comparison of procedural characteristics in the two groups.
|
Variables
|
GROUP dTRA
|
GROUP wTRA
|
Total
|
P Value
|
|
Puncture success
|
43(86%)
|
50(100%)
|
93(93%)
|
0.012
|
|
Puncture Attempt
|
|
|
1.00
|
23(46%)
|
40(80%)
|
63(63%)
|
<0.001
|
|
|
2.00
|
11(22%)
|
10(20%)
|
21(21%)
|
|
|
3.00
|
8(16%)
|
0(0%)
|
8(8%)
|
|
|
>3
|
1(2.0%)
|
0
|
1(1.0%)
|
|
Median puncture attempt
|
1.00
|
1.00
|
1.00
|
|
|
Puncture Time (Sec)
|
|
|
<30
|
7(14%)
|
26(52%)
|
33(33%)
|
<0.001
|
|
|
30-60
|
19(38%)
|
21(42%)
|
40(40%)
|
|
|
>60
|
17(34%)
|
3(6%)
|
20(20%)
|
|
Mean puncture time (Sec)
|
73.56±55.52
|
30.06±16.79
|
50.17±45.08
|
<0.001
|
|
Access Success
|
43(86%)
|
50(100%)
|
93(93%)
|
0.012
|
|
Access Switch
|
|
|
Switched to Wtra
|
7(14%)
|
0(0%)
|
7(7%)
|
0.012
|
|
Access time (Sec)
|
|
|
<30
|
1(2%)
|
6(12%)
|
7(7%)
|
0.118
|
|
|
30-60
|
14(28%)
|
39(78%)
|
53(53%)
|
|
|
>60
|
28(56%)
|
5(10%)
|
33(33%)
|
|
Mean Access Time (Sec)
|
94.95±60.02
|
45.7±17.96
|
68.47±49.26
|
<0.001
|
|
Total Procedure Time (Min)
|
45.72±14.81
|
43.24±14.46
|
44.39±14.6
|
0.417
|
|
Fluroscopy Time(Sec)
|
616.51±209.6
|
592.62±228.7
|
603.67±219.22
|
0.603
|
|
Dose Area Product (Gycm2)
|
89.65±37.85
|
83.11±77.66
|
86.13±62.26
|
0.616
|
|
Complications
|
|
|
Hematoma
|
2(4.7%)
|
7(14%)
|
9(9%)
|
0.169
|
Discussion
Studies on dTRA, including meta-analysis have established its feasibility and safety [6-8]. The dTRA has advantages of lower vascular complications and RAO, lesser RA spasm, post procedure pain and hand clumsiness with better hemostasis and favorable ergonomics for both patient and operator [5, 9]. However, in most of these studies, ACS which has increased risk of bleeding is underrepresented. Head-to-head comparative studies of dTRA and wTRA in primary PCI are few. To the best of our knowledge this is thrid such study with the other two havng a sample size of 109 and 292 [10, 11].
In both the dTRA and wTRA groups majority were males 84% and 68% respectively. Here, as with other studies women were underrepresented [12, 13]. Diameter of distal RA is 0.3-0.6 mm smaller compared to wrist [14]. The distal RA size is less in females (2.09 ± 0.38 mm vs 2.27 ± 0.39 mm in males) (p<0.001) [15]. Smaller size and RA spasm might contribute for increased failure in puncture and cannulating the distal RA in females and patients with low BMI [15, 16]. Ultrasound guided punctures might help improve puncturing. Our study had 7 unsuccessful punctures, only 3 of which were females. Further comparative studies focusing on challenges of dTRA in females are warranted.
Puncture and access were successful in 43/50 (86%) in the dTRA group compared to wTRA group where all 50/50 (100%) were successful. This was statistically significant. All 7(14%) of unsuccessful access in dTRA group were switched to wTRA. Our rate of dTRA puncture and access success are like other studies which reported 88- 100% success [17, 18]. However these studies included small number of ACS. In a study of 138 ST elevation myocardial infarction (STEMI) patients access success was 92.8% by dTRA [19]. Conventional wTRA too has a learning curve and a crossover to femoral access in 4-10% among ACS [20]. 100-200 cases have been suggested to achieve a high >94% puncture success rate in dTRA [16]. As with any procedure, dTRA has learning curve that would ease with experience.
Median puncture attempt was one in both the groups. Median puncture attempt of our study is better than the reported median values from various studies. In the ANGIE trial [21] more punctures were needed for arterial access in the dTRA compared with wTRA (median- 2 vs median - 1 p < 0.001). However, data on puncture attempt in studies involving only STEMI, like our study is sparse.
In our study, puncture time among 38% of dTRA was between 30-60 seconds, as compared to wTRA where 52% had puncture time of <30 seconds which was statistically significant. Mean puncture time was 1.2±0.9 min in dTRA and 0.5±0.27 min in the wTRA group which too was statistically very significant. Mean access time was statistically low in wTRA. However, values of our study are more encouraging in both groups compared to previous studies reporting puncture time of 1.19 to 3.9 minutes in dTRA [19,20]. In a study of STEMI mean access time was 2.7 ± 1.6 minutes by dTRA, which is more than our study [19]. Although the puncture time was a concern in ACS, a study of dTRA in STEMI having puncture time less than 5 minutes did not show statistically significant in delay the door to balloon time [10]. Our study had both access time and puncture time well within 5 minutes in all dTRA, proving its feasibility in ACS.
In both groups of the present study, 6 F introducer sheath was used in all access successful cases, none had RA spasm. This is similar to other studies reporting 88.5% procedures with 6F in dTRA [12]. With dTRA, even 7F sheaths are used for chronic total occlusion PCI [22]. However, use of thinner sheaths of 6F in dTRA would be desirable [15].
In our study mean fluoroscopy time and mean DAP in both the dTRA and wTRA groups are comparable, with no significant statistical difference. These results are consistent with recent meta-analysis of 16 studies [23]. There is no concern of increased radiation with dTRA.
Hematoma was the only vascular complication noted among both the groups. It was seen in 2 (4.7%) dTRA and 7(14%) wTRA cases among access successful cases. Studies have shown lower hematoma, RAO and better hemostasis with dTRA [11, 23]. Although our study had lower hematoma in dTRA, this was not statistically significant, as it was not statistically powered enough. Hence larger studies in ACS are required.
Limitations of the study: The sample size was relatively small. Also study could be limited by selection bias as the dTRA groups were included only after confirming a good palpable distal radial pulsation.
Conclusion
Distal radial access offers a promising alternative for both patient and operator. Although puncture and access as represented by puncture success, access success, puncture time and access time are partially more difficult, they have learning curve effect that would ease with experience. The median puncture attempts were similar in both the distal radial access and conventional radial access groups. The total procedure time, fluoroscopy time and dose area product were similar in both groups, confirming the safety of dTRA. The only access site complication was hematoma, which was less in the distal radial access group, however the difference was not statistically significant. Thus, the dTRA offers to be safe and feasible with advantages of better hemostasis in ACS. However further extensive studies and knowledge sharing are required to further explore this potential alternative to conventional radial access.
Acknowledgement
We express our gratitude to Ms Mridula Vellore, Sr. Research Assistant (scientific writer) for the invaluable guidance in finalizing the manuscript.
Conflicts of interests
Authors declare that there is no conflict of interest.
References
[1] Valgimigli M, Gagnor A, Calabro P, Frigoli E, Leonardi S, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. The Lancet. 2015; 385:2465–2476.
[2] Sinha SK, Jha MJ, Mishra V, Thakur R, Goel A, et al. Radial artery occlusion–incidence, predictors and long–term outcome after transradial catheterization: clinico–Doppler ultrasound–based study (RAIL–TRAC study). Acta Cardiol. 2017; 72:318–327.
[3] Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention. 2017; 13:851–857.
[4] Sgueglia GA, Di Giorgio A, Gaspardone A, Babunashvili A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiovasc. Interv. 2018; 11:2113–2119.
[5] Sgueglia GA, Lee BK, Cho BR, Babunashvili A, Lee JB, et al. Distal radial access: consensus report of the first Korea–Europe transradial intervention meeting. JACC Cardiovasc Interv. 2021; 14:892–906.
[6] Roghani–Dehkordi F, Hashemifard O, Sadeghi M, Mansouri R, Akbarzadeh M, et al. Distal accesses in the hand (two novel techniques) for percutaneous coronary angiography and intervention. ARYA Atheroscler. 2018; 14:95.
[7] Cai G, Huang H, Li F, Shi G, Yu X, et al. Distal transradial access: a review of the feasibility and safety in cardiovascular angiography and intervention. BMC Cardiovasc. Disord. 2020; 20:1–2.
[8] Hamandi M, Saad M, Hasan R, Megaly M, Abbott JD, et al. Distal versus conventional transradial artery access for coronary angiography and intervention: a meta–analysis. Cardiovasc Revasc Med. 2020; 21:1209–1213.
[9] Sharma AK, Razi MM, Prakash N, Sharma A, Sarraf S, et al. A comparative assessment of Dorsal radial artery access versus classical radial artery access for percutaneous coronary angiography–a randomized control trial (DORA trial). Indian Heart J. 2020; 72:435–441.
[10] Lee OH, Kim Y, Son NH, Roh JW, Im E, et al. Comparison of distal radial, proximal radial, and femoral access in patients with ST–elevation myocardial infarction. J Clin Med. 2021; 10:3438.
[11] Kitanoski D, Postadzhiyan A, Velchev V, Stoyanov N, Zimbakov Z, et al. Comparison of distal radial with conventional radial access in patients with ST–segment elevation myocardial infarction, undergoing primary percutaneous coronary intervention. Interv Cardiol. 2021; 14:449–453.
[12] Eid–Lidt G, Rodríguez AR, Castellanos JJ, Pasos JIF, López KEE, et al. Distal radial artery approach to prevent radial artery occlusion trial. JACC Cardiovasc. Interv. 2021; 14:378–385.
[13] Chugh Y, Kanaparthy NS, Piplani S, Chugh S, Shroff A, et al. Comparison of distal radial access versus standard transradial access in patients with smaller diameter radial Arteries (The distal radial versus transradial access in small transradial ArteriesStudy: DATA–STAR study). Indian Heart Jl. 2021; 73:26–34.
[14] Meo D, Falsaperla D, Modica A, Calcagno MC, Libra F, et al. Proximal and distal radial artery approaches for endovascular percutaneous procedures: anatomical suitability by ultrasound evaluation. Radiol Med. 2021; 126:630–635.
[15] Deora S, Sharma SK, Choudhary R, Kaushik A, Garg PK, et al. Assessment and comparison of distal radial artery diameter in anatomical snuff box with conventional radial artery before coronary catheterization. Indian Heart J. 2022; 74:322–326.
[16] Roh JW, Kim Y, Lee OH, Im E, Cho DK, et al. The learning curve of the distal radial access for coronary intervention. Sci Rep. 2021; 11:13217.
[17] Kim Y, Ahn Y, Kim I, Lee DH, Kim MC, et al. Feasibility of coronary angiography and percutaneous coronary intervention via left snuffbox approach. Korean Circ J. 2018; 48:1120.
[18] Soydan E, Akın M. Coronary angiography using the left distal radial approach–An alternative site to conventional radial coronary angiography. Anatol J Cardiol. 2018; 19: 243–248.
[19] Kim Y, Lee JW, Lee SY, Bae JW, Lee SJ, et al. Feasibility of primary percutaneous coronary intervention via the distal radial approach in patients with ST–elevation myocardial infarction. Korean J Intern Med. 2021; 36:S53.
[20] Gragnano F, Jolly S, Mehta S, Branca M, van Klaveren DE, et al. Prediction of radial crossover in acute coronary syndromes: derivation and validation of the MATRIX score: The MATRIX score to predict radial crossover. Euro Interv. 2021; 17:e971.
[21] Tsigkas G, Papageorgiou A, Moulias A, Kalogeropoulos AP, Papageorgopoulou C, et al. Distal or traditional transradial access site for coronary procedures: a single–center, randomized study. JACC Cardiovasc Interv. 2022; 15:22–32.
[22] Feng H, Fang Z, Zhou S, Hu X. Left distal transradial approach for coronary intervention: insights from early clinical experience and future directions. Cardiol Res Pract. 2019; 2019:8671306.
[23] Ferrante G, Condello F, Rao SV, Maurina M, Jolly S, et al. Distal vs conventional radial access for coronary angiography and/or intervention: A meta–analysis of randomized trials. JACC Cardiovasc Interv. 2022; 15:2297–2311.